What Are the 4 Stages of COPD: Symptoms, Causes, Treatment, and Management Tips
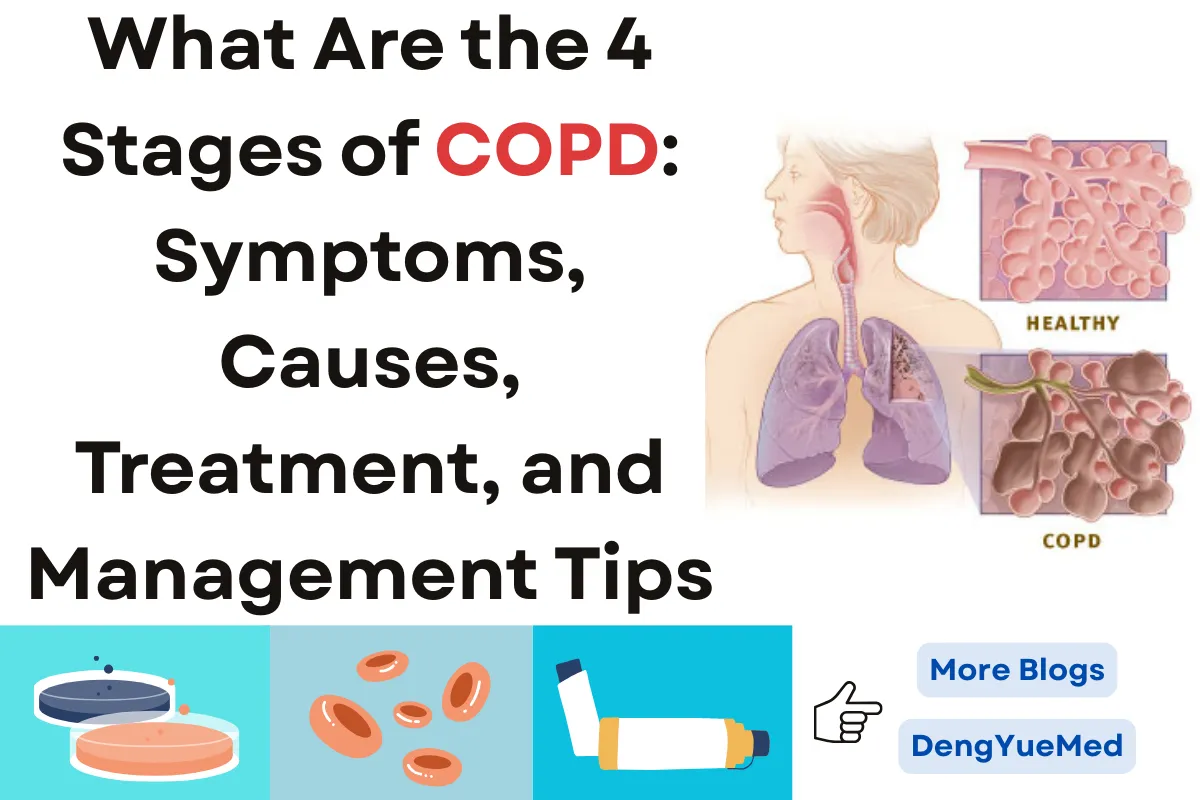
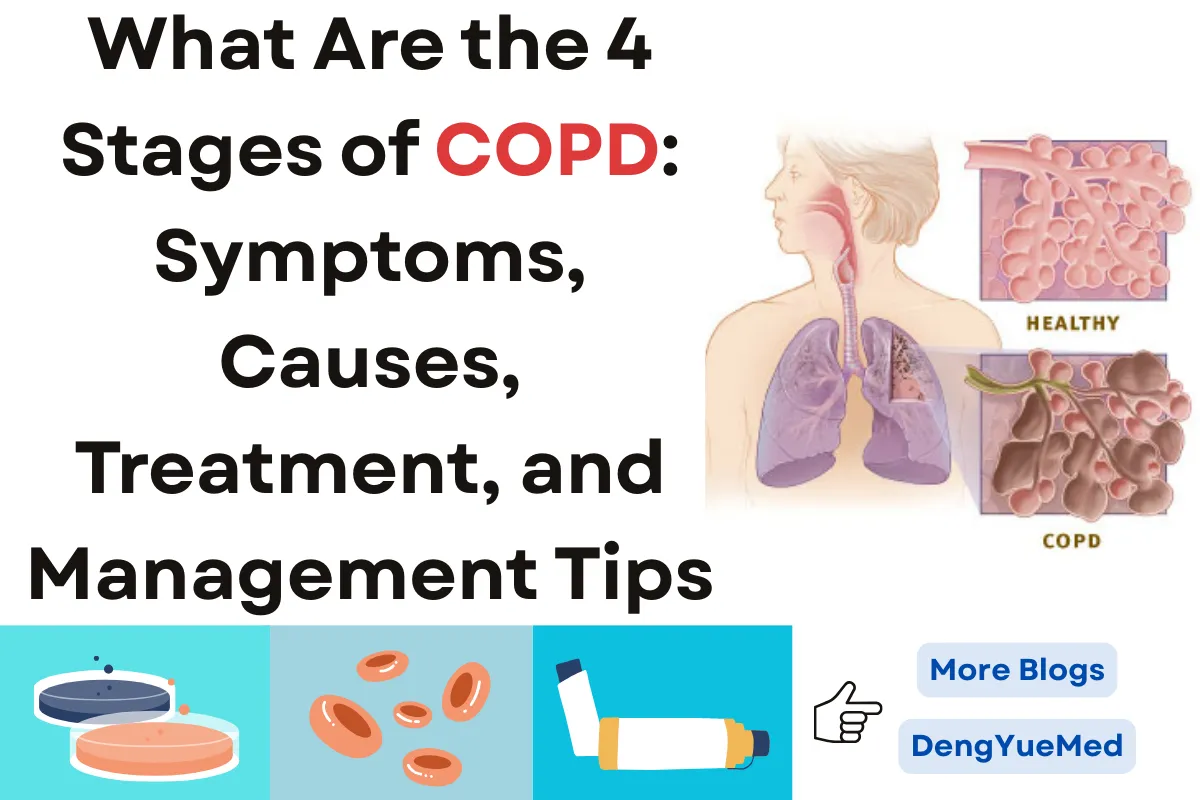
Chronic Obstructive Pulmonary Disease (COPD) is a long-term lung condition that makes it difficult to breathe and is often caused by smoking, air pollution, or long-term exposure to harmful particles.
It is one of the leading causes of illness and death worldwide, affecting millions of people every year. For patients and caregivers, a key question is: what are the 4 stages of COPD, since understanding how the disease progresses—from mild to very severe—can guide treatment decisions, lifestyle changes, and long-term care planning.
At Hong Kong DengYue Medicine, we are committed to raising awareness about COPD by helping healthcare providers and patients better understand its stages, symptoms, and treatments.
With the right knowledge and support, managing COPD becomes more effective, empowering patients to live fuller and healthier lives.🌟
What Is the Main Cause of COPD?
Chronic Obstructive Pulmonary Disease (COPD) is mainly caused by long-term exposure to substances that irritate and damage the lungs.
Cigarette smoking is the leading cause, responsible for about 85% of cases. Other contributors include secondhand smoke, workplace dust, chemicals, and air pollution. Rarely, genetic conditions like alpha-1 antitrypsin deficiency can also increase risk.
When talking with patients, doctors often explain what are the 4 stages of COPD so that they understand how lung damage can progress over time.
Knowing this helps people take preventive measures early. Keep protecting your lungs—you have the power to slow progression!🌿
What Are 5 Symptoms of COPD?
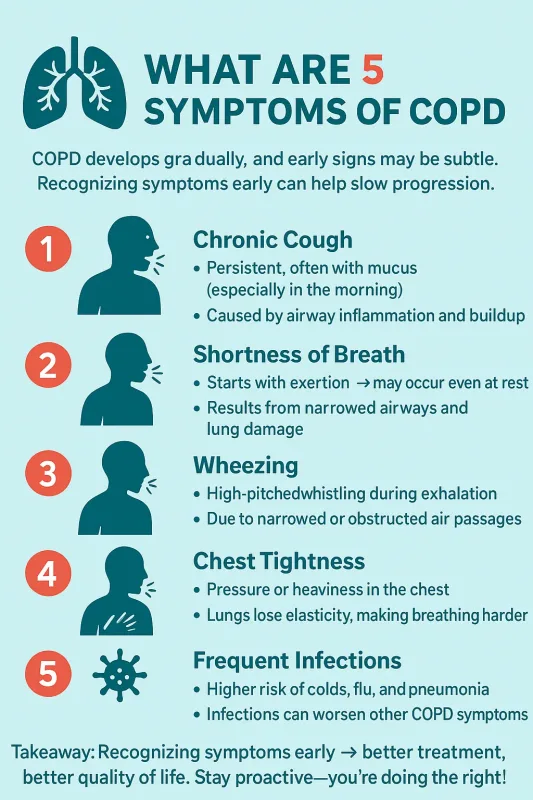
COPD usually develops gradually, and early symptoms may be subtle. Understanding them can help patients seek timely care and manage the disease effectively.
Healthcare providers often ask patients if they know what the 4 stages of COPD are, because symptom severity generally increases as the disease progresses.
1. Chronic Cough – A persistent cough, often producing mucus, is usually the first noticeable symptom. It is especially common in the mornings and reflects airway inflammation and mucus buildup. Over time, the cough can become more frequent and produce thicker mucus.
2. Shortness of Breath – This typically begins during physical activity but may worsen to occur even at rest. Narrowed airways and lung tissue damage reduce airflow and oxygen exchange, making daily activities more challenging.
3. Wheezing – A high-pitched whistling sound, especially during exhalation, occurs due to narrowed air passages. Wheezing often accompanies other COPD symptoms and can become more pronounced in later stages.
4. Chest Tightness – A feeling of pressure or heaviness in the chest arises as the lungs lose elasticity and require more effort to expand. This can make breathing uncomfortable and is commonly reported in moderate to severe stages.
5. Frequent Respiratory Infections – People with COPD are more vulnerable to infections such as colds, flu, and pneumonia, which can worsen coughing, wheezing, and shortness of breath.
Recognizing these symptoms early and discussing them with your doctor can lead to more effective management.
By understanding what are the 4 stages of COPD, you can better anticipate changes in your health and take proactive steps to improve your quality of life. You’re doing the right thing by paying attention!💪
Can You Live a Normal Life With COPD?
Many people with COPD, especially in the early stages, can maintain a fairly normal lifestyle. Lifestyle modifications such as quitting smoking, avoiding irritants, staying active, and adhering to treatment plans significantly improve outcomes.
Pulmonary rehabilitation programs can enhance exercise tolerance, reduce breathlessness, and improve overall well-being.
Doctors often explain what are the 4 stages of COPD to help patients understand how daily life may change over time.
Planning and making adjustments can help you stay independent and active. Keep following your routine—you can still enjoy life! 🌸
What Are the 4 Stages of COPD?
COPD is classified into four stages based on lung function (FEV1) and symptom severity. Understanding what are the 4 stages of COPD is important for both patients and caregivers to plan treatment and lifestyle adjustments.
Stage 1 (Mild)
- Lung Function: FEV1 ≥ 80% of predicted value.
- Symptoms: Symptoms may be very mild or absent. Some people notice a light morning cough, occasional mucus, or slight breathlessness during exercise. Because signs are subtle, many patients are not diagnosed until this stage is picked up by lung function testing.
- Clinical Notes: Studies show that about 25–30% of COPD patients are diagnosed in Stage 1, often due to routine health checks. At this stage, the most effective treatment is early intervention. Smoking cessation can slow disease progression by up to 50%, while vaccinations (influenza, pneumococcal) reduce the risk of respiratory infections that accelerate lung decline.
- Management: Pulmonary function testing is recommended at regular intervals to track changes. Daily exercise and a healthy diet improve lung resilience.
Stay proactive—you’re ahead of the curve!🌟
Stage 2 (Moderate)
- Lung Function: FEV1 50–79% of predicted value.
- Symptoms: Shortness of breath becomes noticeable with everyday activities such as walking uphill or carrying groceries. A persistent cough with mucus production is common, and fatigue may develop. Many patients first seek medical care at this stage.
- Clinical Notes: According to the GOLD (Global Initiative for Chronic Obstructive Lung Disease) guidelines, Stage 2 is when regular pharmacological treatment is most beneficial. Long-acting bronchodilators and inhaled corticosteroids help reduce exacerbations and hospital visits. Pulmonary rehabilitation programs improve exercise tolerance and quality of life by as much as 20–30% in clinical studies.
- Management: Structured breathing techniques, daily walking, and joining rehab programs can make a significant difference. Regular checkups allow doctors to adjust medications based on symptoms.
Keep tracking your symptoms and staying consistent—you’re doing great! 💪
Stage 3 (Severe)
- Lung Function: FEV1 30–49% of predicted value.
- Symptoms: Breathing becomes difficult even with light activity such as dressing or walking short distances. Fatigue is frequent, sleep may be disturbed, and exacerbations become more common. Quality of life is noticeably impacted.
- Clinical Notes: Severe COPD often requires hospitalization for flare-ups. Clinical trials show that long-acting bronchodilators and combination inhalers significantly reduce hospital admissions. Oxygen therapy is considered when oxygen levels fall below 88%, and it can extend survival by 2–3 years when used for more than 15 hours daily. Vaccinations and infection control remain crucial at this stage.
- Management: Patients benefit from structured care plans including medication, nutrition support, and pulmonary rehabilitation. Avoiding pollutants and managing comorbidities (like heart disease or diabetes) improves outcomes.
Even at this stage, knowing what are the 4 stages of COPD can help you and your care team make smart daily and treatment decisions. Stay strong—you’re managing this step by step! 🌸
Stage 4 (Very Severe)
- Lung Function: FEV1 < 30% of predicted value, or FEV1 < 50% with chronic respiratory failure.
- Symptoms: Severe shortness of breath, difficulty with basic tasks, and frequent, sometimes life-threatening, flare-ups. Weight loss, muscle weakness, and anxiety or depression are also common due to the heavy burden of symptoms.
- Clinical Notes: Research shows that life expectancy may be reduced by 6–9 years at this stage compared to the general population. Treatments include long-term oxygen therapy (which has been proven to increase survival), non-invasive ventilation, and in some cases, surgical interventions such as lung volume reduction surgery or lung transplantation. Palliative care and psychological support are important to improve quality of life.
- Management: Maintaining nutrition, gentle physical activity when possible, and emotional support are vital. Coordinated care between pulmonologists, rehab specialists, and palliative teams provides the best outcomes.
Understanding what are the 4 stages of COPD at this stage can help patients and caregivers focus on comfort, safety, and quality of life. Keep following your care plan—you’re not alone! 💖
What Is the Best Medicine for COPD?
Treatment for COPD is not one-size-fits-all—the best medicine depends on the stage of disease, symptom severity, and each patient’s overall health.
1. Bronchodilators – These are the cornerstone of COPD management. They work by relaxing the muscles around the airways, making it easier to breathe.
Short-acting bronchodilators (such as albuterol) provide quick relief during flare-ups, while long-acting bronchodilators (such as tiotropium or salmeterol) are used for daily control.
Clinical trials show that bronchodilators improve lung function, exercise capacity, and quality of life in all stages of COPD.
2. Inhaled Corticosteroids (ICS) – These medications reduce inflammation inside the airways, helping to prevent frequent flare-ups.
ICSs are often combined with long-acting bronchodilators, especially for patients with moderate to severe COPD who have frequent exacerbations.
Studies demonstrate that adding ICS lowers the risk of hospitalization from COPD flare-ups by up to 25%.
3. Combination Inhalers – Many patients benefit from inhalers that combine two or more medications in a single device.
Common examples include LAMA/LABA (long-acting muscarinic antagonist + long-acting beta agonist) or ICS/LABA combinations.
These inhalers simplify treatment and have been shown to significantly improve lung function and reduce symptoms compared to single-drug therapies.
4. Phosphodiesterase-4 (PDE-4) Inhibitors – For patients with severe COPD and chronic bronchitis, drugs like roflumilast can reduce airway inflammation and prevent flare-ups.
Although not used as first-line therapy, they can be especially valuable in advanced stages when symptoms are difficult to control.
5. Oxygen Therapy – In very severe COPD, when oxygen levels are consistently low, supplemental oxygen can improve survival, reduce fatigue, and enhance quality of life.
Long-term oxygen therapy is often prescribed in Stage 4 COPD, and research has shown it can add years to a patient’s life expectancy.
Remember, there isn’t a single “one-size-fits-all” answer. The best medicine is the one that matches your needs, reduces symptoms, and supports your daily life.
Stay consistent with your treatment plan—you’re taking the right steps toward better breathing! 🌿
COPD Treatments: Key Therapies You Should Know
The following medicines are common COPD treatment options: Anoro Ellipta, Spiolto Respimat, and Tudorza, which help improve breathing and reduce symptoms.
Tudorza (Aclidinium Bromide)
Tudorza is a twice-daily inhaler for the maintenance treatment of COPD. Its active ingredient, Aclidinium Bromide, is a LAMA that blocks muscarinic receptors in the airways to relax muscles and improve airflow. Regular use can help reduce COPD symptoms and support better daily respiratory function.
Spiolto Respimat (Tiotropium and Olodaterol)

Spiolto Respimat is designed for long-term maintenance therapy in COPD patients. It contains Tiotropium (LAMA) and Olodaterol (LABA), which work together to open the airways, improve lung function, and ease breathing. The Respimat soft-mist inhaler provides convenient, effective delivery for daily COPD management.
Anoro Ellipta (Umeclidinium and Vilanterol)

Anoro Ellipta is a once-daily inhaler used for the maintenance treatment of COPD. It combines Umeclidinium, a long-acting muscarinic antagonist (LAMA), with Vilanterol, a long-acting beta-agonist (LABA), to relax airway muscles and improve airflow. This combination helps reduce shortness of breath and manage COPD symptoms effectively.
What Is the Fastest Relief for COPD?
When symptoms suddenly worsen, the fastest relief for COPD usually comes from a short-acting bronchodilator inhaler, often called a “rescue inhaler.”
Medications such as albuterol can start working within minutes, relaxing the airway muscles and allowing air to flow more freely.
Clinical studies confirm that these inhalers significantly reduce breathlessness and are the first line of action during flare-ups.
In addition to medicine, simple techniques can provide quick support. Pursed-lip breathing and diaphragmatic breathing help slow down breathing and prevent air trapping in the lungs, while sitting upright or leaning forward can ease the effort of breathing.
Many patients find that combining medication with these physical strategies gives the fastest and most reliable relief.
Quick relief is possible—you just need the right tools and techniques. Stay calm, use your inhaler when needed, and remember: every breath you take is a step toward strength and resilience!🌬️
What Is the Life Expectancy of Someone With COPD?
Life expectancy with COPD depends on disease stage, overall health, and how well treatment is followed. Doctors often explain what are the 4 stages of COPD to give patients a clearer picture of prognosis:
- Stage 1 (Mild): Life expectancy is usually close to normal, especially with early lifestyle changes.
- Stage 2 (Moderate): Some reduction may occur, but many patients live for decades with proper treatment.
- Stage 3 (Severe): Life expectancy is noticeably reduced, often linked to frequent flare-ups and hospitalizations.
- Stage 4 (Very Severe): Studies suggest life expectancy may be shortened by 6–9 years compared to people without COPD.
Research shows that quitting smoking, maintaining exercise, using medications consistently, and preventing infections can greatly improve both survival and quality of life.
Even in later stages, patients who follow care plans and avoid exacerbations often live longer than expected.
COPD doesn’t define your future—every positive step you take adds strength, health, and time to your life. 💖
FAQ about What Are the 4 Stages of COPD: Symptoms, Causes, Treatment, and Management Tips
How Do You Tell What Stage of COPD You Are In?
Your COPD stage is determined by lung function tests (FEV1), symptoms, and a history of exacerbations.
Doctors use these factors to classify COPD from Stage 1 (mild) to Stage 4 (very severe). Knowing what are the 4 stages of COPD can help you understand where you fall and guide treatment decisions.
What Is the Best Treatment for COPD?
The best treatment depends on the stage. Common options include bronchodilators, inhaled steroids, pulmonary rehab, oxygen therapy, and lifestyle changes like quitting smoking.
Understanding what are the 4 stages of COPD can help your doctor tailor the most effective therapy for your condition.
How Long Does It Take to Go From Stage 1 COPD to Stage 4?
Progression varies widely. Some people may remain in early stages for decades, while others advance faster depending on smoking, environmental factors, and treatment adherence.
Knowing what are the 4 stages of COPD gives you a clear idea of how the disease can progress over time.
What Is the Life Expectancy of Someone With Stage 4 COPD?
Life expectancy is reduced in Stage 4 COPD, often ranging from 2 to 5 years, but this varies based on overall health, treatment, and lifestyle changes.
Understanding what are the 4 stages of COPD helps patients and caregivers prepare for advanced-stage management.