Primary Hypertension Treatment Made Simple: What It Is and Key Medication Options Featuring SPH3127 Tablets
Primary hypertension remains one of the most widespread chronic conditions globally.
👉 Currently, approximately 1.2 billion adults are affected by hypertension globally, yet only about 23% achieve blood pressure control targets (<140/90 mmHg).
👉 Among those receiving treatment, over 30% either respond inadequately to existing antihypertensive medications or cannot adhere due to adverse effects, directly contributing to a continued elevated risk of cardiovascular events.
These gaps highlight an urgent need for innovative therapies capable of improving long-term outcomes.
In response to this unmet demand, the newly developed SPH3127 Tablets have now been officially launched.

Next, Dengyuemed will outline the key causes and symptoms of primary hypertension, helping readers understand how this common condition develops.
✅ We will then review the global burden of hypertension and introduce the latest approaches in primary hypertension treatment, highlight the innovative Chinese drug SPH3127.
✅ To explain how its novel mechanism differs from existing antihypertensive options and what this breakthrough could mean for the future of global hypertension management.
Primary Hypertension Causes and Symptoms
🌐 Primary hypertension (also known as essential hypertension) is the most common type of high blood pressure, accounting for the majority of hypertension cases worldwide.
It is not caused by a single disease but develops gradually due to a combination of genetic and environmental factors over many years.
🤔 Because most patients experience no obvious symptoms in the early stages, it is often referred to as a “silent killer.”
Awareness of primary hypertension symptoms, along with its causes and available primary hypertension treatment options, is especially important for early detection, timely intervention, and long-term blood pressure control.
A Multifactorial Condition
Primary hypertension does not have a single curable cause.Instead, hypertension develops from the long-term buildup of multiple factors.
Based on the 2025 survey, here are the 10 most common contributors to rising blood pressure:
1.Genetics and Family History 👨👩👧👦
- Individuals with a family history of hypertension have a significantly higher risk.
- Multiple genes—not a single gene—contribute to susceptibility, making individuals more sensitive to environmental and lifestyle triggers.
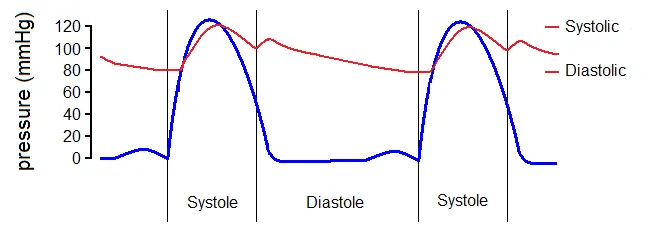
2. Aging and Vascular Stiffness 🧓
- As people age, arterial elasticity decreases and the vessel walls become stiffer, leading to higher systolic blood pressure.
- Elderly individuals are more prone to “isolated systolic hypertension.”
3. Dysregulation of the Renin–Angiotensin–Aldosterone System (RAAS) 🩸
- Overactivation of the RAAS promotes vasoconstriction and sodium–water retention, both of which raise blood pressure.
- Some individuals are genetically more responsive to RAAS stimulation.
4. Sympathetic Nervous System Overactivity 🧠
- Chronic stress, anxiety, poor sleep, and neuroendocrine conditions can increase sympathetic tone, contributing to sustained blood pressure elevation.
5. High Sodium Intake and Poor Diet 🥣
- High salt consumption is a major modifiable risk factor, especially in salt-sensitive individuals.
- Diets high in saturated fats, processed foods, and excessive calories contribute to weight gain and metabolic alterations.
6. Overweight/Obesity and Metabolic Dysregulation 🦵
- Blood pressure rises proportionally with increased body weight.
- Central (visceral) obesity is associated with insulin resistance, chronic inflammation, and other mechanisms that promote hypertension.
7. Excessive Alcohol Consumption and Smoking 🚬
- Chronic heavy drinking raises blood pressure.
- Smoking damages blood vessels and accelerates atherosclerosis, significantly increasing cardiovascular risk.
8. Obstructive Sleep Apnea (OSA) 🛏️
- Repeated nighttime hypoxia, sympathetic activation, and inflammation from OSA strongly contribute to hypertension development.
9. Medications and External Substances 💊
- Long-term use of corticosteroids, certain NSAIDs, oral contraceptives, antidepressants, and some weight-loss products can elevate blood pressure.
- Illicit drugs or supplements containing stimulants also affect blood pressure regulation.
10. Metabolic and Endocrine Factors 🔎
- Conditions like insulin resistance and metabolic syndrome commonly coexist with primary hypertension.
- Note: Specific endocrine disorders (e.g., primary aldosteronism, pheochromocytoma) cause secondary hypertension but should be ruled out during diagnosis.
Symptoms and Clinical Signs
1. Most Patients Have No Symptoms (“Silent Killer”)
- Primary hypertension usually presents with no noticeable symptoms.
- Many individuals discover elevated blood pressure incidentally during routine physical exams.
- Regular monitoring is essential, especially for those with risk factors such as family history, obesity, smoking, excessive alcohol intake, or metabolic disease.
2. Possible Non-Specific Symptoms (When BP Is High or Fluctuating)
- Headache (often occipital or worse in the morning)
- Dizziness or light-headedness
- Palpitations (fast or irregular heartbeat)
- Fatigue or general weakness
- Blurred or transient vision changes
- Shortness of breath (especially with exertion or if heart failure is present)
These primary hypertension symptoms are non-specific and usually occur only when blood pressure is significantly elevated or complications arise.
3. Warning Symptoms of Severe Hypertension or Hypertensive Emergency
Seek immediate medical attention if any of the following primary hypertension symptoms:
- Severe headache, vomiting, mental confusion, or sudden neurological deficits (possible stroke)
- Severe chest pain or chest tightness (possible myocardial ischemia or aortic dissection)
- Marked shortness of breath (possible acute heart failure)
- Sudden visual loss or field defects (retinal hemorrhage or edema)
- Rapid decline in kidney function (reduced urine output, swelling)
These may indicate a hypertensive crisis requiring urgent blood pressure reduction and organ protection.
4. Chronic Organ Damage from Long-Term Uncontrolled Hypertension
Persistent high blood pressure can injure multiple organs, leading to:
- 🫀 Heart: left ventricular hypertrophy, heart failure, coronary artery disease, atrial fibrillation
- 🧠 Brain: ischemic or hemorrhagic stroke, cognitive decline, increased dementia risk
- 👱 Kidneys: chronic kidney disease, proteinuria, progression to end-stage renal disease
- 👁️ Eyes: retinal arteriosclerosis, hemorrhage, vision impairment
- 🩸 Large arteries: atherosclerosis, aortic disease
Primary Hypertension vs Secondary Hypertension
What is primary hypertension?
Unlike secondary hypertension, it does not originate from a single disease. Instead, it develops gradually due to a combination of genetic factors, aging, lifestyle, and environmental influences.
Diagnosis is based on persistent blood pressure levels that meet the standard classification thresholds.
According to widely recognized guidelines, the primary hypertension BP range generally begins at:
- SBP ≥ 130 mmHg or DBP ≥ 80 mmHg (Stage 1)
- SBP ≥ 140 mmHg or DBP ≥ 90 mmHg (Stage 2)
Because primary hypertension progresses slowly and is often asymptomatic in early stages, long-term management is essential.
👉 This is where evidence-based primary hypertension treatment protocol plays a key role.
Such protocols typically include lifestyle modifications (salt restriction, weight control, exercise, limiting alcohol intake) combined with antihypertensive medications when necessary—such as ACE inhibitors, ARBs, calcium channel blockers, diuretics, or newer therapeutic options.
What is secondary hypertension?
Secondary hypertension refers to high blood pressure caused by a specific and identifiable underlying condition.
Unlike primary hypertension—which develops gradually and has no single clear cause—secondary hypertension results from diseases or physiological abnormalities that directly elevate blood pressure.
Common causes include chronic kidney disease, renal artery stenosis, endocrine disorders (such as primary aldosteronism or Cushing’s syndrome), obstructive sleep apnea, and certain medications.
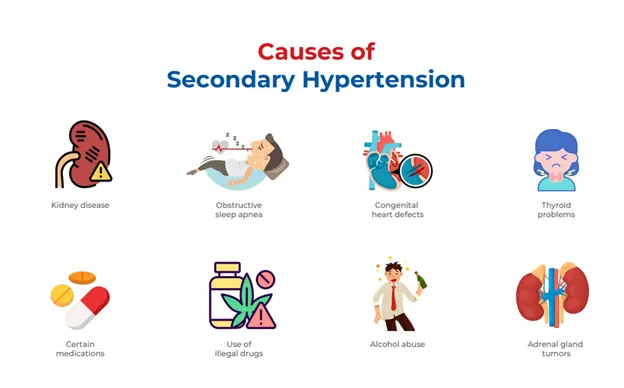
Patients with secondary hypertension often experience a more abrupt onset of elevated blood pressure or unusually high readings that are difficult to control with standard therapies.
Because the condition is driven by an underlying disease, effective management focuses on treating the root cause, which may lead to significant improvement or even normalization of blood pressure.
Identifying secondary hypertension is crucial because its treatment approach differs fundamentally from that of primary hypertension.
💡 By comparing the two, the biggest distinction lies in cause and treatment strategy:
- Secondary hypertension focuses on eliminating the underlying disease.
- Primary hypertension requires individualized, long-term treatment protocols and regular blood pressure monitoring.
Global Burden and What is the Latest Primary Hypertension Treatment?
Primary hypertension remains a major global health challenge, affecting more than 1.2 billion adults worldwide.
As the most common form of hypertension, it progresses silently and contributes to a high burden of cardiovascular diseases—including stroke, coronary artery disease, heart failure, and kidney damage.
🔎 Despite well-established primary hypertension treatment guidelines, global blood pressure control rates remain low, highlighting the need for improved therapeutic strategies and more effective primary hypertension drug options.
Global Burden of Primary Hypertension
Many patients fail to reach the recommended Primary hypertension BP range, even when treated with standard medications.
Factors such as poor adherence, drug intolerance, multi-drug requirements, and individual variability all contribute to inadequate control.
As populations age and lifestyle-related risk factors increase, the demand for simplified, well-tolerated, and innovative primary hypertension treatment options continues to grow.
What Is the Latest Primary Hypertension Treatment?
Current treatment guidelines emphasize several first line drug for primary hypertension categories, including ACE inhibitors, ARBs, calcium channel blockers, and thiazide diuretics.
These remain foundational in the primary hypertension treatment protocol.
However, real-world evidence shows that a significant proportion of patients still struggle to achieve stable BP control, even with combination therapy.
This therapeutic gap has accelerated the development of next-generation drugs designed to target blood pressure regulation more effectively, with better tolerability and longer-lasting effects.
✨ Among these emerging innovations, SPH3127 tablets have attracted increasing attention.
Clinical Trials of SPH3127
💊 As a novel investigational primary hypertension drug, SPH3127 aims to provide a more precise and consistent control of blood pressure while addressing limitations seen in traditional RAAS-based therapies.
Early clinical evidence has shown promising outcomes:
- Effective, Consistent Blood Pressure Reduction
SPH3127 demonstrates significant reductions in both SBP and DBP, with stable 24-hour BP control—an important advantage for patients who struggle to maintain values within the Primary hypertension BP range.
- Fewer RAAS-Related Side Effects
Compared with ACEIs and certain ARBs, SPH3127 shows a favorable safety profile with a reduced risk of cough, dizziness, or electrolyte imbalance.
- Suitable for Once-Daily Dosing
Pharmacokinetic data support convenient long-acting administration, improving adherence—an essential part of effective primary hypertension treatment.
- Benefits in Hard-to-Control Hypertension
Some studies indicate that SPH3127 may be effective in individuals who show inadequate responses to existing first line drug for primary hypertension classes, thereby expanding its potential clinical value.
How SPH3127 Works: A Novel Mechanism Compared to Existing Hypertension Drugs
SPH3127 introduces an innovative mechanism that differentiates it from current RAAS inhibitors:
- Multi-Target Optimization of RAAS Activity
Rather than acting at a single point in the RAAS pathway, SPH3127 delivers a more balanced regulatory effect—resulting in smoother vascular relaxation, reduced sodium retention, and improved BP stability.
- No Bradykinin Accumulation
In contrast to ACEIs, SPH3127 avoids bradykinin buildup, reducing cough and angioedema risks.
- Stable, 24-Hour BP Control
Its long-acting pharmacologic profile ensures more consistent daily control—an essential component of modern primary hypertension treatment protocols.
- Potential Cardiovascular Protective Effects
Preclinical research suggests additional benefits on endothelial function and inflammation, potentially expanding its role beyond simple BP lowering.
As these challenges persist and the limitations of existing therapies become increasingly evident, the search for safer, more effective, and globally scalable solutions has intensified.
✨ This shift in unmet clinical needs has paved the way for next-generation antihypertensive innovations—among which SPH3127 has emerged as a particularly promising breakthrough.
The Global Impact of China’s Innovative Drug SPH3127 on Hypertension Treatment
As global hypertension rates continue to rise, the need for safer, more effective, and better-tolerated treatments has become increasingly urgent.
SPH3127, a novel antihypertensive drug developed in China, represents an important milestone in this landscape.
With its innovative mechanism, SPH3127 offers a potential solution for patients who respond poorly to existing therapies or experience significant side effects.
Early clinical data suggest that it may provide more stable blood pressure reduction, improved tolerability, and broader therapeutic potential compared to traditional regimens.
As China’s biopharmaceutical innovation gains global recognition, SPH3127 is emerging as a promising candidate to reshape treatment standards, expand therapeutic options, and strengthen China’s presence in the international cardiovascular drug market.
Conclusion
‼️ Hypertension—especially primary hypertension—remains a critical therapeutic area where unmet clinical needs persist.
Traditional first-line therapies are effective but not flawless, creating opportunities for new mechanisms, improved safety profiles, and more stable 24-hour blood pressure control.
The successful launch of SPH3127 not only marks a major breakthrough for China in the cardiovascular field but also reflects the overall momentum of China’s R&D ecosystem toward global innovation.
☀️ It brings new therapeutic options to the field of cardiovascular disease.
As the global pharmaceutical landscape continues to evolve, China’s innovation-driven drug development is accelerating, with more breakthrough therapies entering international markets.
This global expansion reflects not only scientific progress but also the growing ambition of Chinese biopharma companies to contribute solutions to major global health challenges.
✨ At DengYue Medicine, we will continue to follow these advancements closely, providing professional insights into emerging treatment options, global research trends, and breakthroughs shaping the future of hypertension management.
FAQ about Primary Hypertension Treatment
What are the early signs of pH?
Early signs of primary hypertension are usually absent, but some people may have mild headaches, dizziness, or palpitations.
The best way to detect it early is regular blood pressure checks.
What is primary and secondary hypertension?
There are two main types of hypertension: primary (essential) and secondary.
Primary hypertension is due to a combination of genetics, lifestyle, and age, while secondary hypertension has an identifiable cause, such as kidney or adrenal gland issues.
What are the 4 types of hypertension?
Types of hypertension include resistant hypertension, isolated systolic hypertension, and malignant hypertension
Is primary hypertension reversible?
Primary hypertension cannot be fully reversed in the true sense, as it has no single identifiable cause and is often linked to long-term factors such as genetics, age, metabolism, and lifestyle.
However, blood pressure levels can be “reversed” back to the normal range.