How Long Can Someone Live With Lung Cancer? Facts, Hope, and Factors That Influence Survival
“How long can someone live with lung cancer?” The question is often the first and most daunting one that arises after a diagnosis.
It carries an immense emotional weight, and the search for an answer can feel overwhelming.
It is crucial to understand from the outset that there is no single, universal answer.
Lung cancer survival is not determined by a simple statistic but by a complex interplay of factors unique to each individual.
Dengyuemed explained that “what statistics provide is a broad picture—a general framework based on large groups of people.
They are a starting point for understanding prognosis, not a definitive prediction for any one person.”
The most encouraging news in oncology today is that the landscape of lung cancer treatment has been transformed. Decades of research have yielded remarkable advancements, turning what was once considered a near-uniformly fatal diagnosis into a manageable condition for many and even a curable one for some.
This article will delve deep into the factors that influence life expectancy, from cancer stage and type to groundbreaking treatments
and personal health factors, aiming to provide a comprehensive, evidence-based, and hopeful perspective.
Understanding the Numbers: Survival Rates Explained
When discussing life expectancy, doctors often refer to “survival rates.” The most commonly used is the 5-year relative survival rate.
This statistic, often sourced from large databases like the Surveillance, Epidemiology, and End Results (SEER) Program,
indicates the percentage of people with a specific cancer who are alive five years after their diagnosis compared to people in the general population.
It is important to remember that these numbers are based on data from people who were treated at least five years ago and may not reflect the latest advancements.
The SEER database categorizes lung cancer into three broad stages:
- Localized: The cancer is confined entirely to the lung.
- Regional: The cancer has spread to nearby lymph nodes or structures.
- Distant: The cancer has metastasized to distant organs like the brain, bones, or liver.
According to the latest data, the 5-year relative survival rates for all types of lung cancer combined are approximately:
- Localized: 65%
- Regional: 37%
- Distant: 9%
- All Stages Combined: 28%
While these figures may seem stark, they represent a significant improvement over past decades and form a baseline from which we can explore the nuances that make every patient’s journey different.
The Most Critical Factor: Cancer Stage at Diagnosis
The stage at which lung cancer is diagnosed is the single most powerful predictor of survival. This is why global health initiatives heavily emphasize early detection.
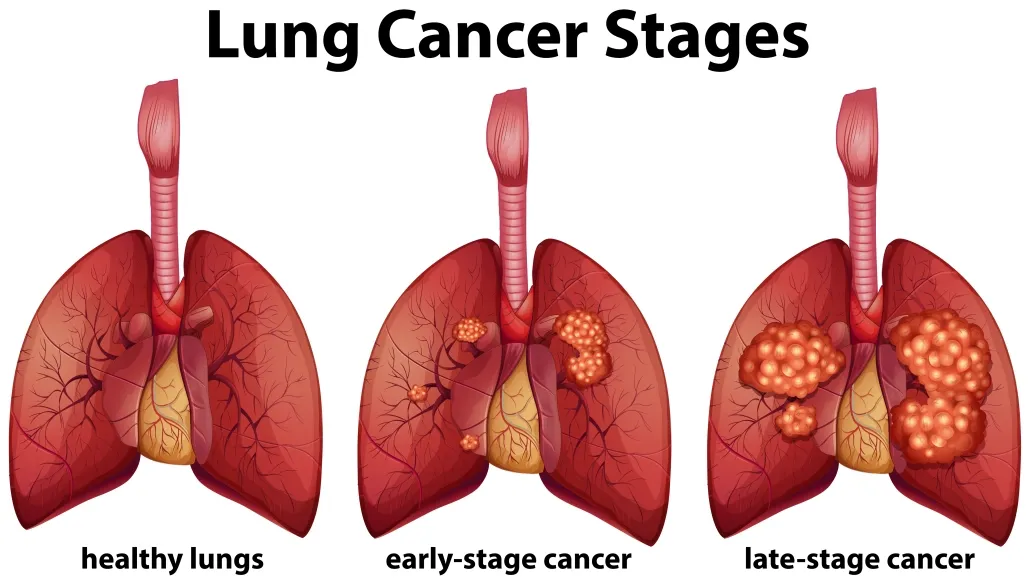
Early-Stage (Localized) Lung Cancer
When lung cancer is detected in Stage I or II, it is typically small and contained within the lung. At this stage, the primary goal is often cure.
- Stage I: For very small tumors (Stage IA), the 5-year survival rate can be 80-90% after surgical resection. For slightly larger Stage I tumors, rates are still very favorable, often above 70-80%.
- Stage II: This stage may involve larger tumors or limited spread to nearby lymph nodes. Survival rates are lower than Stage I but still strong, often ranging from 50-60% with aggressive treatment, which typically includes surgery followed by chemotherapy.
The message here is unequivocal: early detection saves lives.
Low-dose computed tomography (LDCT) screening is recommended for high-risk individuals (e.g., long-term heavy smokers over 50).
This screening has been proven to reduce mortality from lung cancer by detecting it at an earlier, more treatable stage.
Locally Advanced (Regional) Lung Cancer
Stage III lung cancer is a complex and heterogeneous group where the cancer has spread to lymph nodes in the center of the chest but not to distant organs. Treatment is more complex, often involving a combination of chemotherapy, radiation therapy, and sometimes immunotherapy or surgery.
Survival rates vary widely within this stage but have improved dramatically with modern protocols.
With aggressive multimodal treatment, 5-year survival rates can range from 20% to 40%, and in some specific subgroups, even higher.
This area has seen significant progress thanks to immunotherapy.
Advanced (Distant) Metastatic Lung Cancer
Stage IV lung cancer means the cancer has spread to other parts of the body. Until recently, the prognosis for this stage was poor. However, the outlook has changed fundamentally.
While the overall 5-year survival rate is around 9%, this number is rising rapidly and does not tell the whole story.
New treatments are allowing a subset of patients with metastatic disease to live for many years with a good quality of life.
The goal in Stage IV is increasingly shifting from purely palliative to long-term disease management.
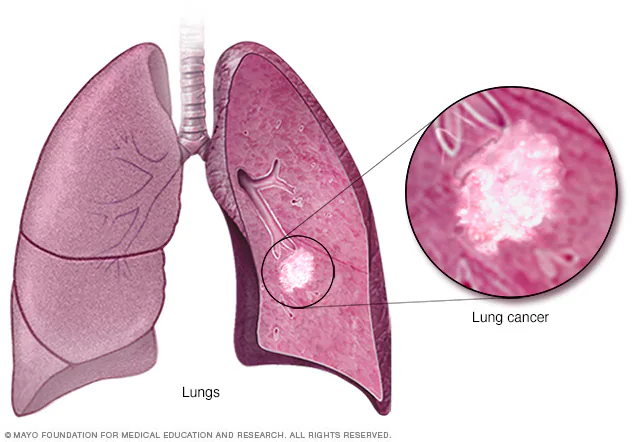
The Impact of Lung Cancer Type: NSCLC vs. SCLC
The type of lung cancer is another critical determinant of survival and treatment.
Non-Small Cell Lung Cancer (NSCLC)
Accounting for about 80-85% of all cases, NSCLC is the most common type.
It includes subtypes like adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
NSCLC tends to grow more slowly than SCLC. The survival rates discussed above primarily reflect outcomes for NSCLC.
Small Cell Lung Cancer (SCLC)
Making up about 10-15% of cases, SCLC is a more aggressive form that grows and spreads rapidly.
It is strongly linked to smoking. SCLC is typically categorized as either:
- Limited-Stage: Cancer is confined to one side of the chest. With chemotherapy and radiation, the 5-year survival rate is about 25-30%.
- Extensive-Stage: Cancer has spread widely throughout the body. The prognosis is more challenging, but the 5-year survival rate has improved from less than 2% to nearly 10% in recent years due to the addition of immunotherapy to first-line chemotherapy
Game Changers: How Modern Treatments Are Redefining “How Long Can Someone Live With Lung Cancer?”
When patients and families ask, “How long can someone live with lung cancer?”
The answer today is fundamentally different than it was a decade ago.
This shift is driven by breakthroughs in targeted therapy and immunotherapy, which are helping many patients live longer, higher-quality lives.
The question of life expectancy with lung cancer is now met with more hope and more personalized answers than ever before
Targeted Therapy
For a significant subset of patients, the question of “how long can you live with lung cancer?” is now addressed through genetic testing.
Targeted therapies are oral drugs designed to attack cancer cells with specific “driver mutations,” offering a more precise attack with fewer side effects than chemotherapy.
The presence of these mutations allows for highly effective, personalized treatment. For example, drugs like Iressa (Gefitinib) are used to treat patients whose tumors have mutations in the EGFR gene. Similarly, Rozlytrek (Entrectinib) is effective against cancers with specific alterations in the NTRK or ROS1 genes.
Iressa (Gefitinib) – NSCLC | HongKong DengYue Medicine
- Generic Name/Brand Name: Gefitinib / Iressa®
- Indications: NSCLC
- Dosage Form: Tablet
- Specification: 250 mg × 10, 30 tablets/box
Rozlytrek (Entrectinib) – NSCLC | HongKong DengYue Medicine
- Generic Name/Brand Name: Entrectinib / Rozlytrek ®
- Indications: NSCLC
- Dosage Form: Capsules
- Specification: 100 mg , 200 mg × 30 capsules/box
For patients with these mutations, targeted therapies have been transformative.
They can often control the cancer for years, turning a once-devastating diagnosis into a chronic condition.
Immunotherapy
Immunotherapy has dramatically changed the outlook for how long patients can live with advanced lung cancer.
It works by unleashing the patient’s own immune system to fight the cancer.
Immunotherapy has led to unprecedented long-term survival for a portion of patients with advanced lung cancer. Studies now show that approximately 15-20% of advanced NSCLC patients treated with immunotherapy can live for five years or longer—a milestone that was once exceedingly rare. These patients are effectively achieving long-term remission.
Conclusion: A Message of Cautious Optimism
So, how long can someone live with lung cancer? The answer is more hopeful today than ever before.
The journey is no longer defined by a single statistic but by a dynamic and evolving landscape of personalized medicine.
The key takeaways are:
- Stage Matters Most: Early detection through screening offers the best chance for a cure.
- Type and Biology are Key: Knowing the specific type and genetic profile of the lung cancer (including testing for biomarkers like EGFR, NTRK, and ROS1 to determine eligibility for drugs like Iressa or Rozlytrek) is essential for selecting the most effective treatment.
- Innovation is Real: Targeted therapies and immunotherapy have fundamentally altered the prognosis for thousands of patients, offering the potential for long-term survival even with advanced disease.
- You are More Than a Statistic: Personal factors, including your overall health and mindset, are powerful contributors to your outcome.
HKDengyuemed emphasized that if you or a loved one is facing lung cancer with treatment, engage in open, honest conversations with your oncology team.
Ask about biomarker testing, discuss all treatment options—including clinical trials—and focus on building a strong support system.
FAQ about How Long Can Someone Live With Lung Cancer
What are the four stages of lung cancer?
Stage II (“stage 2”): The disease may have spread to your lymph nodes near your lungs.
Stage III (“stage 3”): It has spread further into your lymph nodes and the middle of your chest.
Stage IV (“stage 4”): Cancer has spread widely around your body.
How long can you live with stage 4 lung cancer?
The average life expectancy for stage 4 lung cancer patients is 4-13 months, but some people may go on to live for 10 years or more.
How fast does lung cancer grow?
Experts say it takes approximately three to six months for most lung cancers to double in size.
What are the symptoms of end-of-life lung cancer?
Symptoms that are common towards the end of life in lung cancer include pain, dyspnoea, delirium, and respiratory secretions.