A Safer Approach to HDAC Inhibition: Chidamide (Epidaza) for Lymphoma and Breast Cancer
In the field of oncology, relapsed or refractory peripheral T-cell lymphoma (PTCL) and endocrine therapy resistance in HR-positive advanced breast cancer remain two major clinical challenges.
- PTCL is highly aggressive and prone to relapse, leaving many patients with limited treatment options after conventional chemotherapy.
- Similarly, patients with HR-positive breast cancer almost inevitably develop resistance after long-term endocrine therapy, resulting in fewer subsequent treatment choices and a decline in quality of life.
It is in response to these significant unmet medical needs that chidamide(Epidaza/
Hiyasta)—an innovative drug independently developed in China—has emerged.
💊 As the world’s first oral subtype-selective histone deacetylase (HDAC) inhibitor, chidamide exerts its therapeutic effects through a unique epigenetic regulatory mechanism, offering a novel treatment approach for both lymphoma and breast cancer.
✨ Today, Epidaza for lymphoma and breast cancer represents a meaningful advance in the management of these difficult-to-treat malignancies.
🤔 What makes chidamide truly distinctive? And how does it differentiate itself from traditional therapies and other drugs within the same class?
In the following sections, we will take a closer look at the scientific foundation and clinical value of chidamide, exploring why it has attracted growing attention in the global oncology landscape.
This article is provided by Hong Kong DengYue Medicine, aiming to share professional insights into innovative oncology therapies.
Mechanistic Innovation—From “Broad-Spectrum Bombardment” to “Precision Unlocking”
The success of chidamide is no coincidence; it is rooted in profound innovations in its mechanism of action.
Unlike traditional anticancer therapies, Epidaza has pioneered an entirely new therapeutic paradigm.
✨ Rather than relying on indiscriminate “broad-spectrum bombardment” of tumor cells, it achieves precision unlocking of specific cancer types through carefully selected molecular targets and intelligently designed mechanisms.
👉 This chapter takes an in-depth look at the two breakthrough mechanistic innovations that define chidamide’s unique role in modern oncology.
Understanding the Breakthrough: Targeting HDAC at the Core
To fully appreciate the revolutionary significance of chidamide, one must begin with its molecular target.
👉 The primary target of chidamide is histone deacetylase (HDAC)—a family of enzymes that play a central role in epigenetic regulation.
HDACs function as key regulators of chromatin structure and gene transcription.
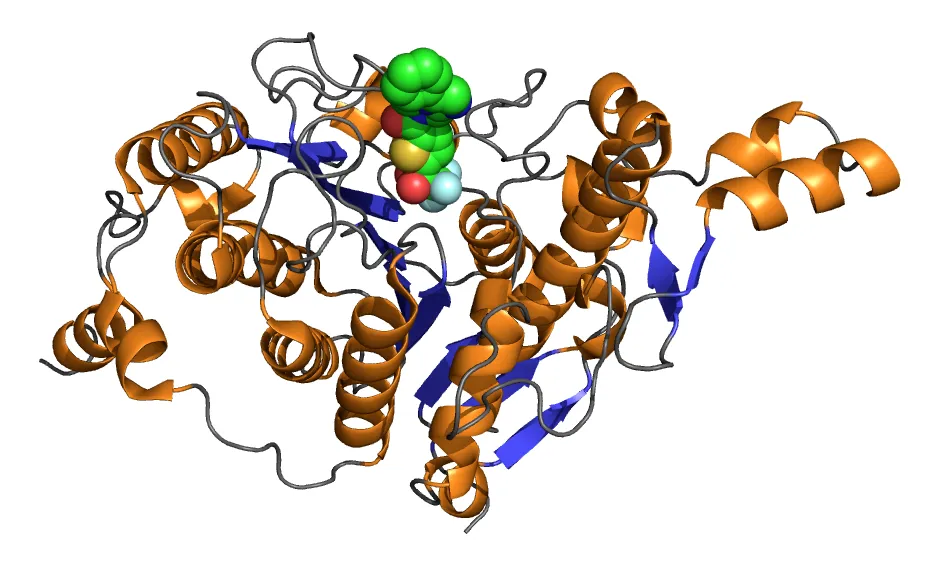
In cancer cells, aberrant overactivation of HDACs acts like a “genetic lock” on DNA, tightly silencing critical tumor suppressor genes and allowing malignant cells to proliferate unchecked.
- Limitations of Traditional HDAC Inhibitors
Conventional HDAC inhibitors, such as vorinostat and romidepsin, adopt a broad-spectrum inhibition strategy.
They indiscriminately suppress multiple HDAC subtypes across both Class I and Class II families. While this “carpet-bombing” approach can produce antitumor activity, it comes at a high cost.
Clinically, these agents are frequently associated with:
- 🫀 Significant cardiotoxicity, including QT interval prolongation
- 🩸 Pronounced hematologic toxicity
- 🥱 Severe and persistent fatigue syndromes
Such safety concerns have substantially limited their long-term clinical use and patient tolerability.
- Chidamide’s Precision Breakthrough
The development team behind Epidaza pursued a fundamentally different approach.
As the world’s first approved oral subtype-selective HDAC inhibitor, Epidaza functions more like a precision-guided intelligent weapon than a blunt therapeutic tool.
Guided by its rational chidamide structure, it selectively targets HDAC subtypes that play a truly critical role in tumor initiation and progression:
- Precise targeting of Class I HDACs: Chidamide selectively inhibits HDAC1, HDAC2, and HDAC3, which are predominantly localized in the nucleus and directly regulate key genes involved in cell cycle control and apoptosis.
- Focused inhibition of a specific Class IIb subtype: Epidaza also targets HDAC10, a subtype closely associated with tumor-specific signaling pathways and metabolic regulation.
This highly selective targeting strategy represents a transformative advance and delivers two major advantages:
- Focused therapeutic efficacy: By precisely inhibiting HDAC subtypes that serve as core drivers in the development and progression of PTCL and breast cancer, Hiyasta more effectively reactivates silenced tumor suppressor genes while avoiding unnecessary interference with non-essential targets.
✅ This enables a highly focused and mechanism-driven antitumor effect, a defining feature of the chidamide mechanism of action.
- Optimized safety profile: Chidamide deliberately avoids inhibition of Class IIa HDACs (such as HDAC4, HDAC5, HDAC7, and HDAC9), which are closely linked to cardiotoxicity.
✅ This conscious design choice significantly reduces the cardiac risks commonly associated with traditional HDAC inhibitors, markedly broadening the therapeutic window and allowing patients to receive long-term, stable treatment.
✨ This revolution in target selectivity is not merely a technical breakthrough; it represents a fundamental evolution in oncology treatment philosophy—shifting from the pursuit of “comprehensive inhibition” to the pursuit of precise regulation.
Dual Mechanisms of Action: A Multidimensional Antitumor Strategy Beyond “Unlocking Genes”
The scientific value of chidamide extends far beyond simply “unlocking” silenced genes. Across different tumor contexts, Epidaza demonstrates an impressive multi-layered and intelligently coordinated mechanism of action, achieving a transformative leap from epigenetic regulation to comprehensive tumor biology remodeling.
- A Triple Synergistic Attack in PTCL
In relapsed or refractory peripheral T-cell lymphoma (PTCL), chidamide establishes a complete three-dimensional therapeutic framework:
1️⃣ First Dimension: Direct Antitumor Activity
Through selective inhibition of HDAC1, HDAC2, and HDAC3, chidamide effectively reverses abnormal histone deacetylation in PTCL cells.
This leads to the reactivation of key silenced tumor suppressor genes—such as p21, PUMA, and BIM—thereby directly inducing programmed cell death in malignant cells.
2️⃣ Second Dimension: Immune Microenvironment Remodeling
This represents one of the most distinctive and innovative aspects of chidamide’s mechanism:
- Enhanced immune recognition: Chidamide significantly upregulates the expression of MHC class I and II molecules on tumor cell surfaces, effectively placing a “high-visibility label” on cancer cells and markedly improving cytotoxic T-cell recognition and killing efficiency.
- Relief of immune suppression: By modulating immune cell function and cytokine networks within the tumor microenvironment, Hiyasta reduces the production of immunosuppressive cytokines such as IL-10 and TGF-β, partially releasing the “brakes” that tumors impose on the immune system.
- Activation of innate immunity: Studies have shown that Hiyasta can enhance natural killer (NK) cell activity, creating a multilayered immune surveillance and antitumor attack network.
3️⃣ Third Dimension: Synergy in Combination Therapy
Building on its unique immunomodulatory effects, chidamide Epidaza strong synergy when combined with immune checkpoint inhibitors, such as PD-1/PD-L1 inhibitors.
By simultaneously enhancing tumor antigen presentation and alleviating immune suppression, this combination strategy addresses two critical steps in antitumor immunity, offering a novel and promising therapeutic option for lymphomas that are refractory to conventional treatments.
- Reversing Treatment Resistance in Breast Cancer
When confronted with the complex challenge of endocrine therapy resistance in HR-positive breast cancer, Hiyasta demonstrates its unique strength as a true “resistance-reversal strategist.”
Epigenetic Reprogramming to Restore Therapeutic Sensitivity: Under prolonged endocrine treatment pressure, breast cancer cells gradually establish new epigenetic barriers that allow them to adapt and survive.
👉 Chidamide is able to reverse this process by re-opening chromatin structure, thereby restoring tumor sensitivity to aromatase inhibitors and effectively reactivating the clinical efficacy of endocrine therapy.
- Precise Modulation of Estrogen Receptor (ER) Signaling
- Inhibition of oncogenic pathways: Hiyasta downregulates the transcriptional activity of estrogen receptor alpha (ERα), reducing the expression of downstream pro-survival genes.
- Activation of tumor-suppressive pathways: At the same time, it upregulates estrogen receptor beta (ERβ), which is associated with potential tumor-suppressive functions.
This finely tuned bidirectional regulation shifts the ERα/ERβ balance, fundamentally disrupting the estrogen-dependent signaling network that sustains tumor growth.
The mechanistic innovation of chidamide represents a new pinnacle in targeted therapy.
Through precise target selection, it avoids the toxicity pitfalls associated with traditional HDAC inhibitors, while its intelligently coordinated, multi-layered mechanisms of action enable differentiated and precise antitumor effects across diverse tumor environments.
✨ This individualized, biology-driven treatment strategy not only reflects advances in pharmacology but also marks a fundamental shift in oncology—from a “one-size-fits-all” approach to truly tailored therapy.
Clinical Evidence — Building a Foundation of Trust Through Efficacy Data
Innovative mechanisms must ultimately withstand the rigorous validation of clinical trials. Beyond its scientifically sound design, Epidaza has delivered compelling results across a series of well-conducted clinical studies.
This chapter presents robust clinical evidence demonstrating the real-world therapeutic value of chidamide for lymphoma and breast cancer, focusing on its performance in two major indications. 🔻
Peripheral T-Cell Lymphoma: Breakthrough Efficacy Reshaping the Treatment Landscape
In 2014, Epidaza was approved in China for the treatment of relapsed or refractory peripheral T-cell lymphoma (PTCL).
This approval was based on a landmark pivotal Phase II clinical study enrolling patients who had failed conventional chemotherapy—an area of profound unmet medical need.
- Key Efficacy Outcomes:
- Objective Response Rate (ORR): 28%
- In a heavily pretreated, refractory patient population where standard therapies had already failed, nearly one-third of patients achieved significant tumor reduction. At the time, this represented a breakthrough outcome in a setting with very limited effective treatment options.
- Median Duration of Response (DoR): 9.9 months
- Patients who responded were able to maintain disease control for nearly one year, translating into a meaningful extension of progression-free survival.
- Sustained Disease Control: When patients achieving stable disease were included, the overall disease control rate exceeded 50%, underscoring the durability of clinical benefit.
- Safety Profile:
- Manageable adverse events
- The most common Grade 3–4 adverse events were thrombocytopenia (28%) and neutropenia (26%).
- Favorable cardiac safety
- In contrast to earlier HDAC inhibitors, Hiyasta demonstrated a very low incidence of cardiotoxicity.
- No treatment-related deaths
- Importantly, no deaths directly attributable to Hiyasta occurred during the trial period.
HR-Positive Advanced Breast Cancer: A Breakthrough Option After Endocrine Resistance
In 2019, based on the pivotal Phase III ACE trial, chidamide combined with exemestane was officially approved for the treatment of HR-positive, HER2-negative, postmenopausal advanced breast cancer that had relapsed or progressed after prior endocrine therapy.
This trial established Chidamide as the first epigenetic agent to reverse endocrine resistance in solid tumors, further strengthening the clinical value of Epidaza for lymphoma and breast cancer.
| Efficacy Endpoint | Chidamide + Exemestane | Placebo + Exemestane | Statistical Difference |
| Median PFS | 7.4 months | 3.6 months | HR = 0.56, 44% risk reduction |
| ORR | 18% | 9% | 100% increase |
| CBR | 46% | 34% | Significant improvement |
- PFS Doubling Effect: The median PFS in the combination arm was more than twice that of exemestane alone, translating into an average extension of nearly four months before disease progression.
- Improved Depth of Response: The doubling of ORR indicates that the combination not only delays disease progression but also enables a substantially higher proportion of patients to achieve meaningful tumor shrinkage.
- Broad Clinical Benefit: Nearly half of the patients experienced clinical benefit, a particularly notable outcome in the post-endocrine-resistance setting where treatment options are limited.
The clinical data for chidamide not only confirm its therapeutic efficacy, but—more importantly—provide practical and viable solutions for two patient populations with limited treatment options.
In the field of PTCL, Epidaza fills a critical gap for patients with relapsed or refractory disease; in breast cancer, it breaks through the long-standing barrier of endocrine resistance.
✨ These rigorously validated clinical results form a solid foundation for the clinical value of chidamide for lymphoma and breast cancer, offering physicians and patients alike a high level of confidence in its therapeutic potential.
Conclusion: Chinese Innovation in the Era of Precision Medicine
Chidamide represents more than a therapeutic breakthrough—it reflects a new paradigm of Chinese innovation aligned with the global evolution toward precision medicine.
🏢 As highlighted by DengyueMed—a global pharmaceutical supplier, its development showcases how a deep understanding of tumor biology and epigenetic regulation can be translated into clinically meaningful and commercially viable therapies.
From relapsed/refractory PTCL to endocrine-resistant HR+ breast cancer, Epidaza shows that precision epigenetic regulation can unlock new treatment possibilities where conventional approaches fall short.
Its development reflects a strategic evolution: not simply following existing drug classes, but redefining them through selectivity, safety, and clinical relevance.
In the era of personalized oncology, Epidaza stands as a representative example of “Chinese wisdom” in drug innovation—delivering globally meaningful solutions rooted in local scientific breakthroughs, and offering patients, clinicians, and the market a smarter, more sustainable path forward.
FAQ about Chidamide for Lymphoma and Breast Cancer
Is there a link between breast cancer and lymphoma?
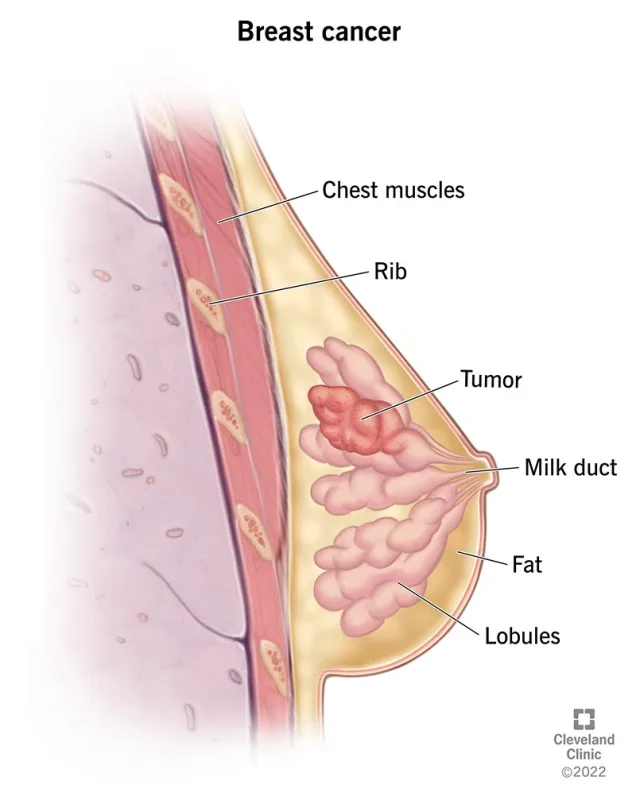
Yes, among women, breast cancer (BC) is the most prevalent type of cancer and the top cause of cancer deaths.
Following chemotherapy or radiotherapy, patients with BC are at greater risk of developing non-Hodgkin lymphoma (NHL), the most prevalent hematological cancer.
Is Chidamide approved by the FDA?
This is an oral pan-HDACI that got FDA approval in 2006 to treat cutaneous T-cell lymphoma (CTCL)
What is the brand name of Chidamide?
Epidaza and Hiyasta
What are CDK 4/6 inhibitors for breast cancer?
CDK4/6 inhibitors are drugs designed to interrupt the growth of cancer cells.