Is Melanoma Cancer Curable? 5 Powerful Facts for Hopeful Recovery

Melanoma cancer is a type of skin cancer that begins in the pigment-producing cells called melanocytes. When these cells grow uncontrollably, they can form tumors and, in advanced stages, spread to other parts of the body.
Although melanoma cancer accounts for a smaller percentage of skin cancer cases, it causes the majority of skin-cancer-related deaths due to its aggressive nature.
Early detection and treatment are critical — when caught early, melanoma cancer can often be cured, offering patients a strong chance for long-term survival.
Understanding these 5 powerful facts about melanoma cancer helps patients and families recognize warning signs sooner, seek timely medical attention, and explore advanced treatment options that improve outcomes.
At Hong Kong DengYue Medicine, we believe that knowledge empowers recovery. By spreading awareness and sharing trusted medical insights, we aim to help patients, caregivers, and healthcare professionals make informed decisions for a healthier, more hopeful future.
Can Melanoma Cancer Be Cured? 5 Empowering Facts That Bring Hope For Recovery
Early Detection Increases Cure Rates
Early detection of melanoma cancer is the single most important factor in achieving a cure. Patients diagnosed with stage I melanoma cancer—where the tumor is less than 1 mm thick—have a five-year survival rate of over 99%, while stage II patients with slightly thicker tumors still have a survival rate above 80%.
Clinical data from large melanoma cancer registries show that removing tumors before they penetrate deeply into the skin or spread to lymph nodes dramatically reduces mortality.
Moreover, advanced imaging and dermoscopy technologies have improved the accuracy of early diagnosis, enabling physicians to detect melanoma cancer at subclinical stages.
Studies also demonstrate that regular skin checks, both by dermatologists and self-exams, significantly increase the chance of catching melanoma cancer early, with one study showing a 30–50% higher detection rate in patients under regular surveillance.
Early surgical excision remains the gold standard, and for most early-stage melanomas, it is curative. Remember, early detection is your first step towards recovery. Stay vigilant and proactive. 💪
Immunotherapy Offers Long-Term Survival
Immunotherapy has transformed the prognosis for advanced melanoma patients. Immune checkpoint inhibitors, such as ipilimumab and nivolumab, work by unleashing the body’s immune system to attack melanoma cells.
Clinical trials have shown that combination therapy can lead to long-term survival in over 50% of patients with stage III or IV melanoma cancer, with some patients remaining disease-free for more than 10 years.
Single-agent PD-1 inhibitors like pembrolizumab and toripalimab have demonstrated objective response rates of 40–45%, with durable responses lasting several years.
Additionally, immunotherapy has proven effective in patients who failed previous treatments, offering hope even in advanced or metastatic disease.
These therapies are now standard-of-care for high-risk melanoma cancer and have fundamentally shifted the landscape from short-term palliation to potential cure.
Your strength and the power of modern medicine are formidable allies. 🌟
Targeted Therapies Improve Outcomes
For patients with BRAF V600 mutations, targeted therapies offer a precise, effective approach. Drugs such as dabrafenib and trametinib inhibit the mutated BRAF pathway, which drives tumor growth.
Clinical trials demonstrate that combination BRAF and MEK inhibitor therapy leads to overall response rates of 70–75%, with median progression-free survival extending to 11–12 months in advanced melanoma cancer.
Importantly, these therapies also delay the development of resistance compared with single-agent treatment.
For patients with metastatic disease, targeted therapy can shrink tumors quickly, reduce symptoms, and sometimes make previously inoperable tumors resectable.
Emerging real-world data suggest that early initiation of targeted therapy in combination with immunotherapy may further enhance long-term survival.
Embrace the advancements in personalized medicine—your path to recovery is becoming clearer. 🧬
Clinical Trials Pave the Way for New Treatments
Participation in clinical trials is essential for accessing novel therapies and improving long-term outcomes. Recent trials exploring new checkpoint inhibitors, combination immunotherapies, and oncolytic viruses have reported response rates of 50–60% in heavily pretreated patients.
For example, combining a PD-1 inhibitor with an experimental CTLA-4 agent achieved complete response in nearly 25% of participants, while more than half experienced significant tumor shrinkage.
Trials also highlight the potential of neoantigen vaccines and cellular therapies to induce durable immune responses, even in patients with aggressive or metastatic melanoma cancer.
These results are transforming previously grim prognoses into manageable or potentially curable scenarios and offer insights into which patient populations benefit most from each therapy.
By considering clinical trials, you become a part of the journey toward better treatments for all. 🔬
Supportive Care Enhances Quality of Life
Supportive care is a critical, yet sometimes overlooked, component of melanoma cancer management. Psychological support, nutritional guidance, pain management, and rehabilitation have all been shown to improve treatment adherence, reduce complications, and enhance overall survival.
Clinical studies indicate that patients who participate in structured supportive care programs have 20–30% higher quality-of-life scores and better physical functioning compared with those receiving standard care alone.
Moreover, supportive interventions help manage immune-related side effects from immunotherapy, reduce fatigue, and improve mental resilience during treatment.
Integrating palliative and supportive care early, even alongside curative treatment, ensures that patients maintain strength, confidence, and motivation throughout their cancer journey.
You are not alone on this journey—support is available to help you thrive. 🤝
Who Is Most At Risk For Melanoma?
Melanoma risk varies greatly based on genetic, environmental, and lifestyle factors. Individuals with fair skin, light eyes, or red or blonde hair are at higher risk because they have less melanin, the pigment that protects against ultraviolet (UV) radiation.
Studies show that people with a history of severe sunburns before age 18 have a twofold increase in melanoma risk later in life.
Family history is another major factor—those with a first-degree relative diagnosed with melanoma face a 50% higher lifetime risk.
Moreover, people with many or atypical moles (more than 50 nevi) are more susceptible. Immunocompromised individuals—such as organ transplant recipients—also show a significantly elevated risk due to reduced immune surveillance.
Finally, frequent use of tanning beds before the age of 30 increases melanoma risk by up to 75%, according to epidemiological data.
Awareness is protection—knowing your risk helps you act early. 🌞
What Are 5 Signs Of Melanoma?
Recognizing melanoma early depends on identifying suspicious skin changes. The “ABCDE rule” is the most reliable method used by dermatologists worldwide:
- A – Asymmetry: One half of the mole looks different from the other.
- B – Border: Irregular, blurred, or jagged edges may indicate malignancy.
- C – Color: A mix of colors (brown, black, red, blue, or white) is concerning.
- D – Diameter: Lesions larger than 6 mm are more likely to be melanoma.
- E – Evolving: Rapid changes in size, color, or shape are warning signs.
Clinical studies show that over 90% of early-stage melanomas present with at least one of these features.
In rare cases, melanoma can appear as a new lesion rather than a pre-existing mole. Regular self-examination and annual dermatologist visits are essential for early identification.
Check your skin often—your vigilance can save your life. 🕵️♀️
How Long Can You Have Melanoma And Not Know It?
Melanoma can sometimes develop silently over several years before it becomes noticeable. Superficial spreading melanoma, the most common type, may grow slowly along the surface of the skin for months or even years before penetrating deeper layers.
However, nodular melanoma progresses much faster—sometimes in just a few months. A 2023 clinical analysis found that.
Hidden areas, such as the scalp, back, soles of the feet, and nails, can harbor melanoma without being noticed. Because symptom-free progression is possible, routine skin screening and dermoscopy play a vital role in early detection and prevention of metastasis.
Even silent changes matter—stay alert and proactive. 👀
What Happens When You Are Diagnosed With Melanoma?
A melanoma diagnosis triggers a series of careful evaluations to determine the stage and best treatment. The first step is usually a biopsy, where the lesion is examined under a microscope to assess thickness (Breslow depth) and ulceration.
If the melanoma is thicker than 1 mm, doctors often perform a sentinel lymph node biopsy to check for regional spread. Imaging tests such as CT, PET, or MRI may follow for advanced cases.
Based on the results, treatment may include surgical excision, immunotherapy, targeted therapy, or radiation, depending on the stage.
For early-stage melanoma, surgery alone is curative in over 90% of patients. Clinical guidelines emphasize multidisciplinary care, combining oncology, dermatology, and pathology teams to ensure optimal outcomes.
Knowledge brings control—understanding your diagnosis empowers you to fight back. 💪
Melanoma Treatments: Key Therapies You Should Know
Mektovi (Binimetinib)

Mektovi is an MEK inhibitor used in combination with other targeted drugs to treat BRAF V600E or V600K mutation–positive melanoma cancer. It works by blocking key signals that drive tumor cell growth and division.
When paired with a BRAF inhibitor, Mektovi can significantly improve progression-free survival and help control advanced melanoma cancer more effectively.
YERVOY (Ipilimumab)
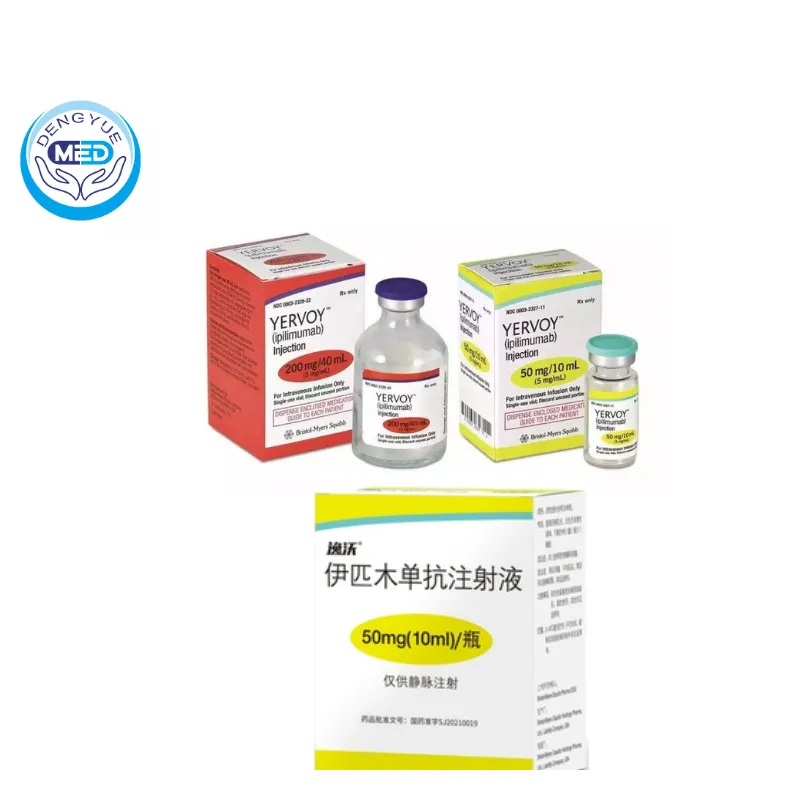
Yervoy is an immune checkpoint inhibitor (CTLA-4 blocker) that boosts the body’s immune system to attack melanoma cells. It helps T-cells stay active longer and enhances immune response against cancer.
Yervoy is often used with nivolumab or other PD-1 inhibitors, offering durable responses for patients with advanced or metastatic melanoma cancer.
Tuoyi (Toripalimab)
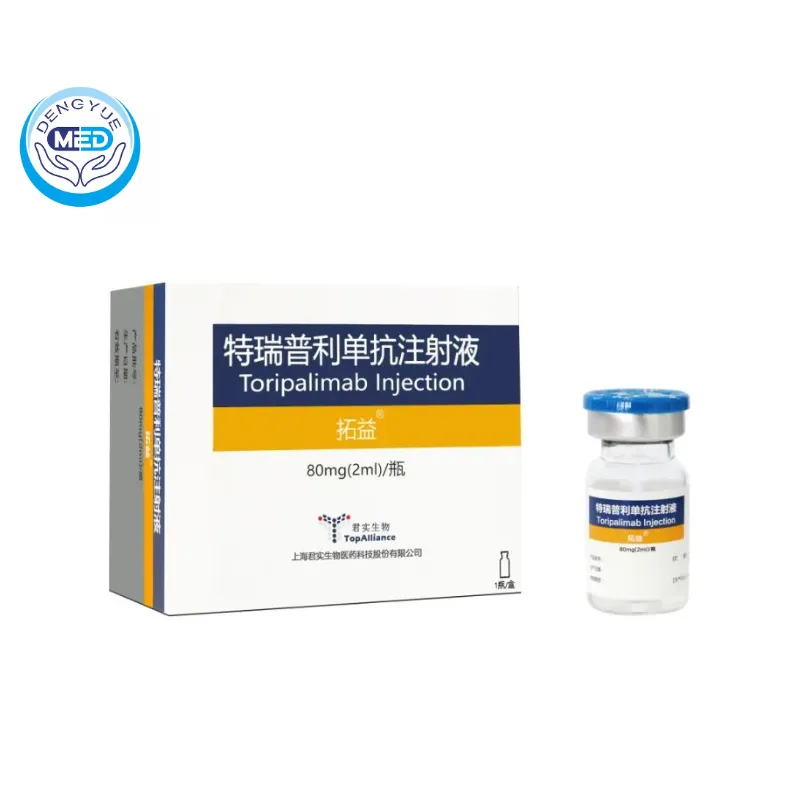
Tuoyi is a PD-1 inhibitor that helps the immune system recognize and destroy melanoma cells by blocking the PD-1/PD-L1 pathway.
Clinical studies have shown that Tuoyi can extend overall survival and reduce tumor size in patients who have progressed after previous treatments, making it a promising immunotherapy option.
Tafinlar (Dabrafenib Mesylate)
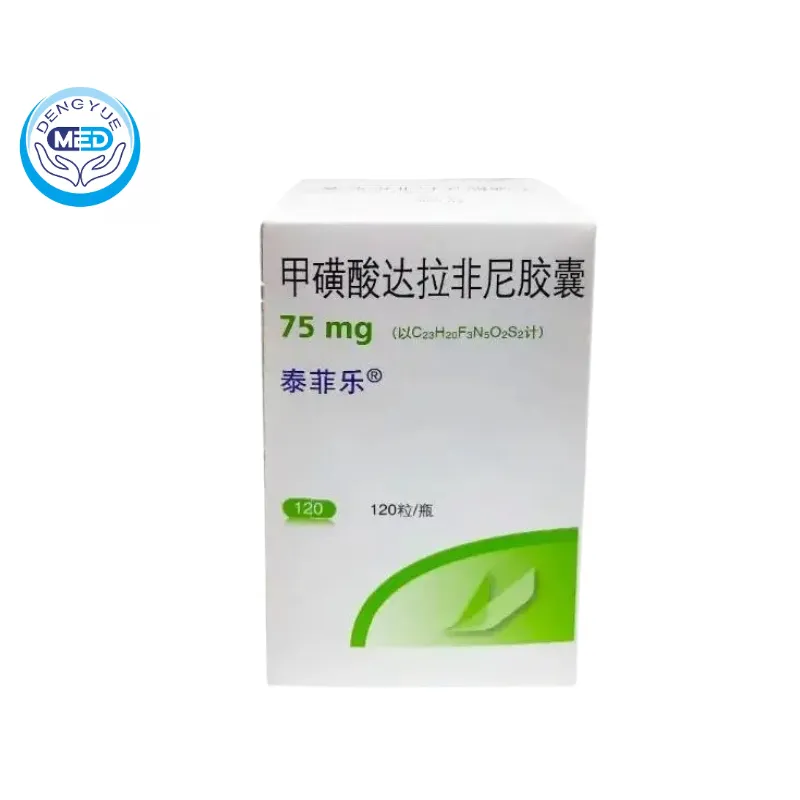
Tafinlar is a BRAF inhibitor designed to target specific genetic mutations that fuel melanoma cell growth. It’s most effective in patients with BRAF V600 mutations.
When combined with MEK inhibitors such as Mektovi or Trametinib, Tafinlar enhances tumor control, delays resistance, and improves long-term outcomes.
Does Melanoma Ever Go Away?
Yes, melanoma can go away—especially when detected and treated early. Stage 0 and Stage I melanomas are almost always curable with surgery, boasting five-year survival rates of 98–99%.
Even some advanced melanomas now show remission with modern therapies. Immunotherapy has achieved complete response rates exceeding 20–30%, where all visible tumors disappear and remain undetectable for years.
Targeted therapy combinations like dabrafenib and trametinib have extended median survival beyond 33 months in metastatic cases, compared to less than 9 months a decade ago.
While recurrence can occur, ongoing follow-up and imaging reduce the risk of late detection. With consistent monitoring and new drugs emerging every year, melanoma “going away” is no longer rare—it’s increasingly possible.
With persistence and progress, recovery is within reach. 🌈
What Is The Survival Rate Of Melanoma?
Survival depends largely on the stage at diagnosis. According to large cohort analyses, the five-year survival rate for localized melanoma (confined to the skin) is 99%, while for regional spread it drops to 71%, and for distant metastases it is approximately 35%.
However, these numbers are improving rapidly due to advances in therapy. Long-term follow-up data from immunotherapy trials show 10-year survival exceeding 50% for patients with advanced disease receiving combined checkpoint inhibitors.
Real-world data also confirm that integrating surgery, immunotherapy, and targeted therapy leads to extended progression-free survival and durable responses.
Melanoma is now one of the few solid tumors where long-term remission is achievable in metastatic cases, reflecting remarkable progress in oncology.
Statistics are improving every year—hope is stronger than ever. 💖
What Kills Melanoma Cells Naturally?
Melanoma cells can be suppressed or destroyed through both medical and natural immune mechanisms. The human immune system, particularly cytotoxic T-cells and natural killer (NK) cells, plays a central role in identifying and eliminating malignant cells.
Certain lifestyle factors can enhance immune efficiency—adequate vitamin D levels, balanced nutrition rich in antioxidants, and regular physical activity support immune surveillance.
Research shows that tumor environments low in glucose or high in oxidative stress can reduce melanoma cell viability.
While no diet or supplement alone can “cure” melanoma, integrative approaches combining medical treatment and immune support have been shown to improve response rates and overall resilience.
Clinical studies highlight that patients with strong immune function respond better to therapies like PD-1 inhibitors.
Nurture your body—it’s your best natural defense. 🌿
FAQ about Is Melanoma Curable? 5 Powerful Facts for Hopeful Recovery
Can You Live 20 Years After Melanoma?
✅ Yes. Many people live 20 years or longer after melanoma cancer, especially when it’s detected early and treated promptly. Survival greatly depends on the stage at diagnosis.
Is Melanoma A Serious Cancer?
⚠️ Yes. Melanoma cancer is one of the most serious types of skin cancer because it can spread quickly to other parts of the body if not caught early.
Can You Have Melanoma For 2 Years And Not Know?
😮 Yes, it’s possible. Melanoma cancer can develop slowly and remain unnoticed for years, especially if it appears in hidden areas or looks like a harmless mole.
What Is Melanoma In Dogs?
🐶 Melanoma in dogs is a type of cancer that starts in pigment-producing cells. It often appears in the mouth, skin, or toes and can spread rapidly if untreated.