When Should You Take Avatrombopag Maleate (Qinganxin)—Precision Solutions for the “Platelet Crisis”
When should you take Avatrombopag Maleate (Qinganxin)?
❗ Platelets, these tiny components in the blood, play a crucial role in the body’s clotting process. When their numbers drop significantly, the body is left without an essential line of defense against bleeding, increasing the risk of hemorrhage.
Now, let us follow Hong Kong DengYueMedicine as we begin with two challenging clinical scenarios and take an in-depth look at this precision treatment option—exploring how Avatrombopag Maleate (Qinganxin) brings new hope to selected patients.
Disease Awareness—Two Challenging Types of “Platelet Crisis”
To understand the value of a therapy, one must first clearly define the challenge it is designed to address.
Avatrombopag primarily targets two clinical scenarios that not only alter laboratory values but also more profoundly reshape a patient’s life trajectory.
Chronic Liver Disease–Associated Thrombocytopenia: When Disease Blocks the “Path” to Treatment
This is not an independent disease but a common complication of advanced chronic liver conditions such as cirrhosis. Its pathogenesis stems from a dual insult:
- 1️⃣ Severe liver dysfunction leads to insufficient synthesis of thrombopoietin (TPO)—a shortage of the “raw material” needed for platelet production
- 2️⃣ Portal hypertension causes hypersplenism, resulting in excessive sequestration and destruction of platelets—an acceleration of “consumption.”
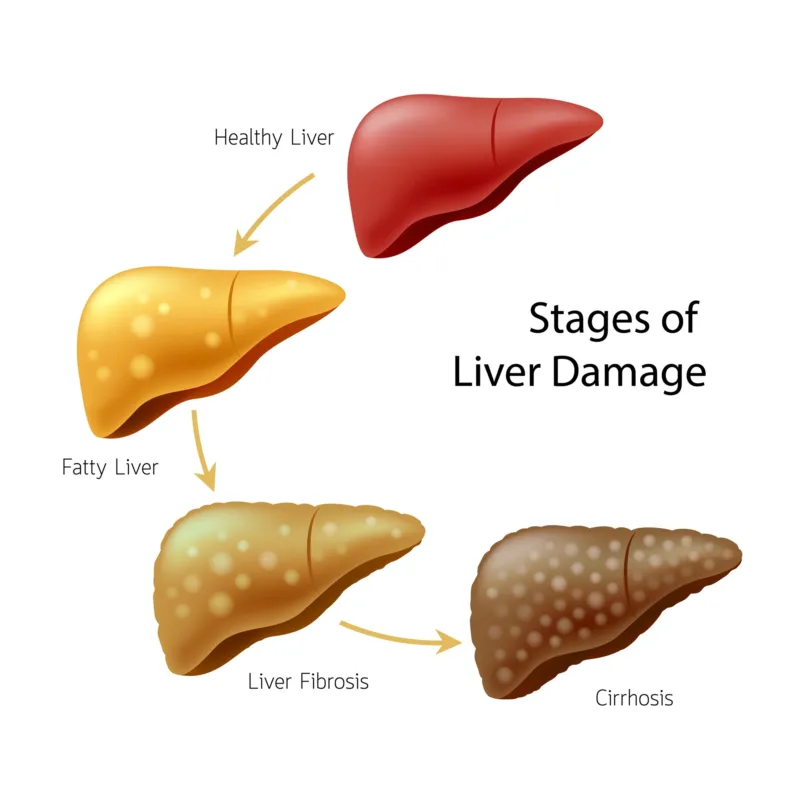
🔬 Clinical data indicate that approximately 70% of patients with cirrhosis develop thrombocytopenia, and about 15% have platelet counts below 50 × 10⁹/L, a level associated with a markedly increased risk of bleeding.
The tangible core dilemma: This condition is more than a number on a lab report—it becomes a literal barrier to treatment.
It renders liver biopsy (the diagnostic gold standard), curative resection or interventional therapies for liver cancer (such as TACE), and even life-saving liver transplantation extremely high-risk, due to the potential for uncontrollable intraoperative or postoperative bleeding.
👉 Clinically, this often leads to a vicious cycle: “Low platelet count prevents surgery → tumor or liver disease progresses → overall condition deteriorates.” As a result, precious windows for intervention are repeatedly missed.
However, traditional approaches such as preoperative platelet transfusion offer only transient benefit, typically lasting hours to days, and may cause allergic reactions, fever, or alloantibody formation that renders subsequent transfusions ineffective.
This represents a passive, symptomatic response—addressing the manifestation rather than the root cause.
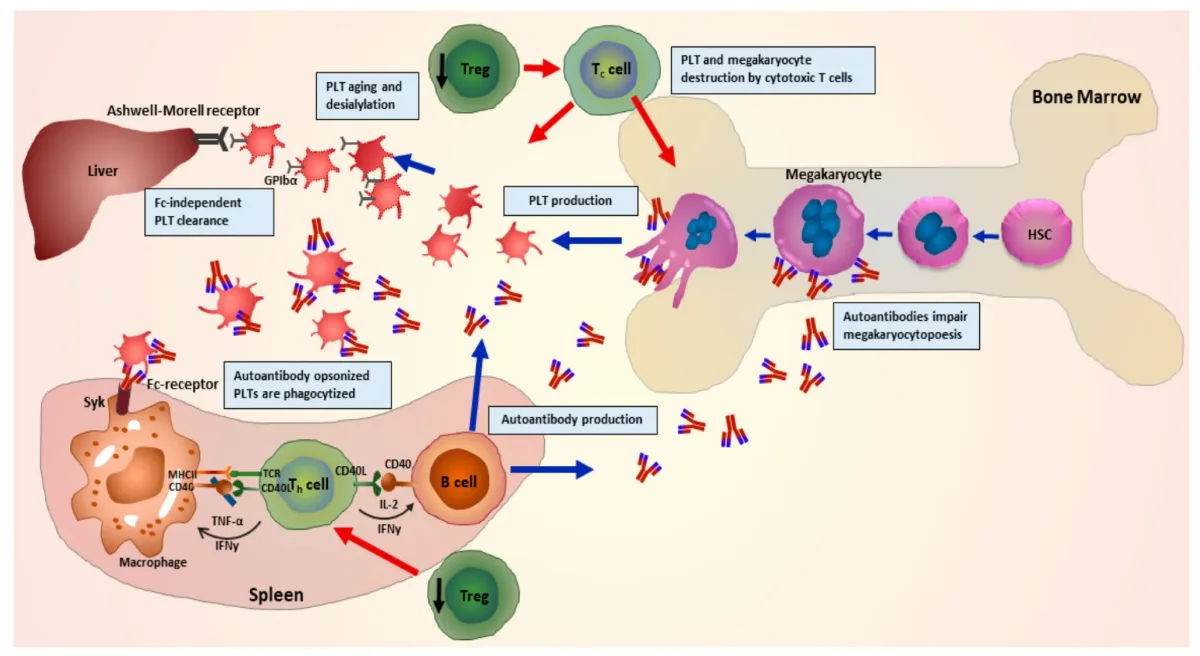
Chronic Primary Immune Thrombocytopenia: A Prolonged Battle Against the Immune System
This is an autoimmune disorder in which the immune system mistakenly identifies platelets as foreign, producing autoantibodies that target them for premature destruction, primarily in the spleen.
At the same time, platelet production in the bone marrow—the body’s “manufacturing plant”—may also be impaired.
Patients live under the constant shadow of bleeding.
☹️ This is evident not only in sudden petechiae, unexplained bruising, gum bleeding, or easy hematoma formation, but also in the fear of severe hemorrhage, where a minor bump may cause joint bleeding, or fluctuations in blood pressure could trigger life-threatening gastrointestinal or intracranial bleeding.
The psychological anxiety and social withdrawal caused by this uncertainty can be as debilitating as the physical symptoms themselves.
🏥 In China, the estimated annual incidence is approximately 65,000 cases, and in patients over 60 years of age, the risk of fatal bleeding is several times higher than in younger individuals, making management particularly challenging.
Under these circumstances, corticosteroids (such as prednisone) remain the cornerstone of first-line treatment.
While effective in some patients, long-term or high-dose use often introduces new problems: weight gain, hyperglycemia, hypertension, osteoporosis, increased infection risk, and mood disturbances.
Many patients face a painful trade-off—”the disease is controlled, but the body suffers“—or develop steroid dependence, with relapse occurring upon dose reduction.
Whether facing urgent surgery for liver disease or enduring a prolonged struggle with ITP, both patient populations confront the limitations—the “ceiling”—of traditional therapies.
When platelet transfusions serve only as temporary measures and steroid-related toxicities become intolerable, clinicians and patients alike call for a solution that can raise platelet counts in a more proactive, sustained, and safer manner.
This is not merely about normalizing laboratory values but about reopening critical therapeutic pathways, restoring control over daily life, and reclaiming safety and dignity.
🤔 As a result, medical focus has turned to a more central question: how can the body’s own platelet-production system be safely and efficiently reactivated? This is precisely the starting point of a new generation of treatment strategies.
Introducing the Treatment Paradigm—A Shift from “Passive Replacement” to “Active Stimulation”
In response to the “platelet crisis” caused by chronic liver disease and immune thrombocytopenia (ITP), the evolution of clinical treatment strategies clearly reflects a deepening understanding of disease biology.
Therapeutic approaches have progressed from simple “replacement of loss” and “suppression of destruction” toward today’s emphasis on precise modulation aimed at restoring physiological function.
➡️ At present, the core strategies for managing thrombocytopenia can be broadly categorized into three approaches, each based on a distinct therapeutic logic and suited to different clinical scenarios.
Passive Replacement—Emergency Platelet Transfusion
This approach represents a form of replacement therapy.
When circulating platelet reserves are critically depleted, platelets are directly collected from healthy donors and transfused into the patient to rapidly replenish platelet counts
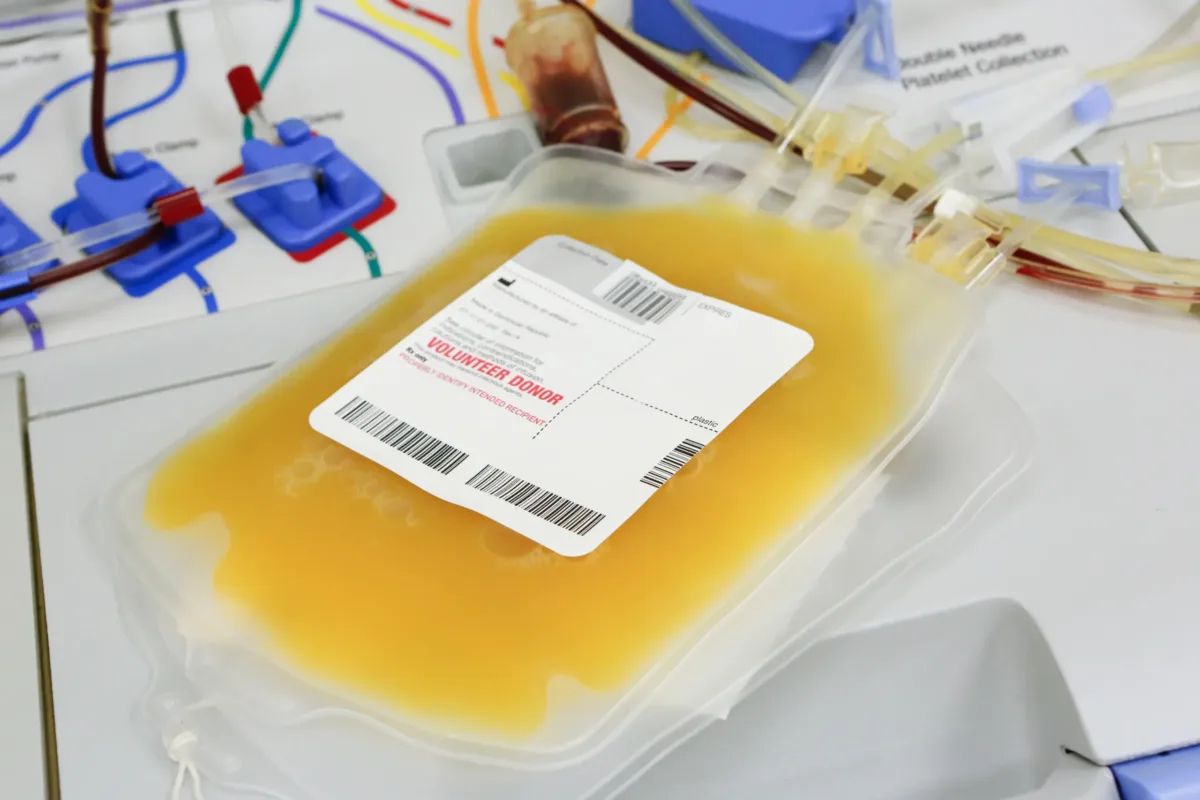
- Effect and limitations:
✨ Its greatest advantage lies in its rapid onset of action, making it a lifesaving intervention in cases of severe, life-threatening bleeding such as intracranial hemorrhage or massive gastrointestinal bleeding.
However, this effect is akin to “borrowed reinforcements”—highly transient in nature.
- Transfused platelets survive in the circulation for only a few days and are quickly destroyed or consumed.
- Repeated transfusions may also lead to fever, allergic reactions, or the development of alloantibodies, progressively reducing efficacy and potentially rendering future transfusions ineffective.
Consequently, platelet transfusion cannot provide the stable platelet support required for elective procedures, nor is it a viable option for the long-term management of chronic disease.
Immunosuppression—Temporary “Ceasefire” Control
This strategy functions as a form of corrective therapy, particularly targeting the autoimmune basis of ITP.
By using corticosteroids and other immunosuppressive agents, it broadly suppresses the overactive immune system responsible for attacking platelets, thereby reducing platelet destruction.
- Effect and limitations:
As the standard first-line treatment for ITP, this approach is effective in a substantial proportion of patients.
However, the cost of “quelling the immune battle” can be significant.
- Long-term or high-dose use is associated with systemic adverse effects that are difficult to ignore, including markedly increased infection risk, osteoporosis, and even osteonecrosis of the femoral head, hyperglycemia, hypertension, weight gain, and mood disturbances.
- More importantly, relapse is common once the dose is tapered or treatment is discontinued, leading to treatment dependence.
In patients with thrombocytopenia secondary to cirrhosis, this strategy is generally ineffective, as immune-mediated destruction is not the primary underlying cause.
Active Stimulation of Production—Restoring Capacity at the Source
This approach represents an incentive-based therapy and embodies the most advanced treatment philosophy to date.
✅ Rather than focusing on platelet loss or destruction, it directly addresses the fundamental problem—insufficient platelet production.
Through the use of thrombopoietin receptor agonists (TPO-RAs), endogenous platelet-producing signals are mimicked or enhanced, directly stimulating megakaryocytes within the bone marrow—the body’s “hematopoietic factory”—to proliferate and differentiate, thereby increasing platelet output at its source.
- Characteristics and clinical positioning:
This strategy offers the greatest potential for disease-modifying benefit.
- It provides potent, sustained, and predictable increases in platelet counts, with a safety profile distinct from that of immunosuppressive therapies and generally more manageable.
- It fills a critical unmet clinical need: offering stable and reliable platelet support for elective procedures in patients with chronic liver disease, while also serving as a long-term maintenance option for patients with ITP, improving quality of life.
❗ In doing so, it marks a true transition from “crisis management” to “steady-state restoration.”
The evolution of treatment strategies has clearly converged on the path of active stimulation of platelet production.
Yet even along this path, different therapeutic options exist. Earlier generations of TPO-RAs, while groundbreaking, were accompanied by practical limitations and clinical concerns.
✨ It was against this backdrop that avatrombopag (brand names: Qinganxin® ), as a representative of the new generation, achieved key breakthroughs through refined molecular design—aiming to deliver a more optimized therapeutic experience and an improved treatment option for patients.
Mechanism of Action — How Does Avatrombopag Maleate (Qinganxin) “Precisely” Stimulate Platelet Production?
The outstanding clinical performance of avatrombopag (brand names: Qinganxin®) is no coincidence.
It is the direct result of a precisely engineered, mechanism-driven design at the molecular level.
To understand how this therapy efficiently and safely accomplishes its platelet-boosting mission—and ultimately informs when should you take avatrombopag maleate—the process can be broken down into three key steps.
Precise Targeting — Identifying the “On Switch” of the Production Line
Within the bone marrow, megakaryocytes are the sole “factories” responsible for platelet production.
➡️ On their surface lies the thrombopoietin receptor (TPO-R)—the critical “on switch” that initiates the entire production process.
Under normal circumstances, endogenous thrombopoietin serves as the natural key to activate this switch.
➡️ However, in many patients, this key is either insufficient in quantity—as seen in Chronic Liver Disease (CLD)—or inefficient in function, as in Chronic Primary Immune Thrombocytopenia (ITP).
As a small-molecule, non-peptide TPO receptor agonist, avatrombopag is designed like a high-affinity, precision-engineered “replica key.”
It binds selectively and stably to the transmembrane domain of TPO-R, effectively mimicking and replacing the impaired endogenous signal, thereby restoring the initiation of platelet production at its source.
Potent Activation — Driving Efficient Intracellular Signaling
Once precisely engaged with the receptor, avatrombopag maleate provides sustained and stable activation, rather than a transient signal.
This activation triggers two pivotal intracellular pathways—the JAK–STAT and MAPK signaling cascades—which serve as the core command systems for platelet generation.
Through signal amplification, megakaryocytes receive a strong and unambiguous directive: accelerate proliferation, differentiation, and maturation.
➡️ As a result, a single megakaryocyte can expand dramatically in size, develop an extensive demarcation membrane system, and segment into thousands of proplatelet structures, laying the groundwork for large-scale platelet release.
Safe Output — Producing Functional Platelets While Avoiding Immune Interference
Mature megakaryocytes extend their cytoplasm into the bone marrow sinusoids, ultimately shedding large numbers of fully functional platelets into the circulation.
Unlike peptide-based TPO receptor agonists (such as romiplostim), avatrombopag maleate tablets share no structural homology with endogenous human proteins.
Consequently, they are far less likely to be recognized as foreign antigens by the immune system.
This design fundamentally minimizes the risk of neutralizing antibody formation, which could otherwise reduce efficacy or even worsen thrombocytopenia.
➡️ In doing so, avatrombopag ensures long-term stability, predictable platelet responses, and a favorable safety profile, addressing a key concern related to avatrombopag side effects in chronic therapy.
Building on this finely tuned mechanistic foundation, the next section will explore how these molecular advantages translate into tangible clinical benefits.
Core Analysis — The Clinical Value of Qinganxin® (Avatrombopag Maleate Tablets)
The precise mechanism and therapeutic advantages of avatrombopag ultimately translate into real-world benefit through Qinganxin® (Avatrombopag Maleate Tablets), a high-quality domestic generic now available in China.
Its clinical value is reflected across three key dimensions: efficacy, safety, and accessibility.
Proven Efficacy: Clinically Validated, Originator-Equivalent
As a generic that has passed China’s consistency evaluation for quality and efficacy, Qinganxin® is therapeutically equivalent to the originator product (Doptelet®).
- Rapid onset: In perioperative use for Chronic Liver Disease (CLD)–associated thrombocytopenia, the standard 5-day regimen significantly increases the proportion of patients achieving target platelet counts (≥50 × 10⁹/L) by Day 8, enabling scheduled procedures to proceed without delay.
- Sustained control: In chronic ITP, Qinganxin® helps maintain platelet counts at safe levels (≥50 × 10⁹/L) during treatment, reducing bleeding risk and improving quality of life.
Strong Safety Profile: Inherited and Optimized
Qinganxin® fully retains the next-generation safety advantages of avatrombopag:
- 🥗 No dietary restrictions: Can be taken with food, improving convenience and long-term adherence.
- 🫁 High hepatic safety: Free of metal-chelation groups, avoiding mechanism-related liver toxicity—especially important for CLD patients.
- 🟢 Non-immunogenic: As a small-molecule, non-peptide agent, long-term use is unlikely to induce neutralizing antibodies, ensuring stable efficacy.
Defining Advantage: A Breakthrough in Accessibility
The greatest clinical and societal value of Qinganxin® lies in its dramatically improved affordability, achieved through domestic production and inclusion in China’s national volume-based procurement program.
- 💰 Equal quality, lower cost: Originator-equivalent efficacy at a significantly reduced price, easing long-term financial burden for patients and healthcare systems.
- 🌐 Broader access: Lower costs remove economic barriers, allowing more patients—especially those in primary care settings—to benefit from advanced TPO-RA therapy.
Qinganxin (Avatrombopag Maleate) – ITP/CLD | HongKong DengYue Medicine
- Generic Name/Brand Name: Avatrombopag Maleate/Qinganxin
- Indications: Thrombocytopenia in Chronic Liver Disease, Chronic Primary Immune Thrombocytopenia
- Dosage Form: Tablet
- Specification: 20 mg × 10 tablets
✨ In summary, Qinganxin® (Avatrombopag Maleate Tablets) preserves the precision mechanism and clinical strengths of next-generation TPO receptor agonists, while transforming an advanced therapy into a safe, effective, and economically accessible option.
Patient Guide — Proper Use and Key Precautions for Qinganxin
After understanding the clinical value of Qinganxin® (Avatrombopag Maleate Tablets), the most practical concern for patients is how to use it safely and correctly to achieve optimal results. Below is a clear and concise patient guide.
1. When Should You Take It? — Two Core Treatment Scenarios
Qinganxin® is not indicated for all causes of thrombocytopenia. It is mainly used in the following two physician-diagnosed clinical settings:
- Perioperative Platelet Support for Elective Procedures
- Eligible patients: Adult patients with chronic liver disease (such as cirrhosis) whose platelet counts are too low to safely undergo scheduled surgery, liver biopsy, or interventional procedures.
- Treatment goal: Short-term elevation of platelet counts to a safe level to allow the planned procedure.
- Typical regimen: Treatment usually starts 10–13 days before the scheduled procedure, taken once daily for 5 consecutive days.
The exact timing must strictly follow the physician’s instructions.
- Long-Term Management of Chronic Primary Immune Thrombocytopenia (ITP)
- Eligible patients: Adult patients diagnosed with chronic primary immune thrombocytopenia who have had an inadequate response to, relapse after, or intolerance to first-line therapies such as corticosteroids.
- Treatment goal: Sustained elevation and maintenance of platelet counts within a safe range to reduce bleeding risk and improve quality of life.
- Typical regimen: Taken once daily on a long-term basis. The usual starting dose is 20 mg (one tablet), with subsequent dose adjustments based on platelet response.
How Should It Be Taken?
- Administration:
- Take once daily, with or without food.
- This is a key advantage of Qinganxin® compared with earlier agents (such as eltrombopag), as there is no need to avoid calcium-, iron-, or magnesium-rich foods, greatly improving treatment convenience and adherence.
- Dose adjustment:
- 🧑⚕️ Always follow your physician’s instructions.
- 🙅♂️ Do not change the dose or discontinue treatment on your own.
- Dosage is adjusted based on regular platelet count monitoring, aiming to maintain platelet levels sufficient to prevent bleeding without excessive elevation (generally ≥50 × 10⁹/L).
Key Precautions — Ensuring Safety and Effectiveness
- Prescription-only use: Qinganxin® must be prescribed and supervised by a hematology or hepatology specialist after comprehensive clinical evaluation.
- Mandatory monitoring:
- Regular platelet count monitoring during treatment is essential.
- It ensures therapeutic effectiveness and helps prevent excessive platelet elevation, which may increase the rare risk of thrombosis. Monitoring is particularly frequent during dose adjustments.
- Special populations:
- 🤰 Use with extreme caution in pregnant or breastfeeding women and in patients with severe hepatic impairment.
- Physicians will carefully weigh potential benefits and risks.
- Potential side effects:
- 😣 Common adverse reactions include headache, fatigue, and nausea, which are usually mild.
- 🫨 Seek immediate medical attention if symptoms such as chest pain, shortness of breath, sudden limb swelling, or sudden visual changes occur, to rule out rare thrombotic events.
✨ The proper use of Qinganxin® begins with clear indications confirmed by a specialist, relies on a once-daily, food-flexible dosing regimen, and depends critically on regular platelet monitoring and close physician–patient communication.
By following this guidance, patients can safely and effectively benefit from this modern targeted therapy.
Conclusion
✅ The introduction of Avatrombopag Maleate Tablets (Qinganxin®) offers patients with chronic liver disease–associated thrombocytopenia and chronic primary immune thrombocytopenia an effective, safe, and convenient oral treatment, featuring no hepatotoxicity or dietary restrictions and representing a meaningful advance in precision-targeted hematologic therapy.”
💴 As a high-quality domestic generic that has passed China’s national quality and efficacy consistency evaluation, and through inclusion in the National Volume-Based Procurement (VBP) program, this therapy has substantially lowered both access barriers and financial burden for patients.
This progress is supported by coordinated efforts across the pharmaceutical value chain, including China pharmacy wholesale suppliers such as DengYueMed——a professional pharmaceutical supply chain service provider.
By strengthening drug distribution and access, such organizations help ensure that high–clinical-value therapies like Qinganxin® are delivered more efficiently and widely to medical institutions at all levels—allowing more patients who need treatment to benefit on time.
FAQ about When Should You Take Avatrombopag Maleate
What is avatrombopag for liver function?
Avatrombopag can be recommended for treating thrombocytopenia in people with chronic liver disease who need planned invasive procedures as an alternative to lusutrombopag.
How to increase platelets in liver cirrhosis?
Several medications can help manage thrombocytopenia in liver cirrhosis.
Types of Medications: Thrombopoietin Receptor Agonists (TPO-RAs): These stimulate the bone marrow to produce more platelets.
Corticosteroids: These can increase platelet counts by reducing the immune system’s destruction of platelets.
How long does avatrombopag take to work?
In clinical studies, platelet counts generally increased within 1 week after starting avatrombopag and decreased within 1 to 2 weeks after discontinuation.
When to take avatrombopag?
Avatrombopag comes as a tablet to take by mouth.
For the treatment of thrombocytopenia in people with chronic liver disease who are scheduled to have a procedure, it is usually taken with food once a day for 5 days, starting 10 to 13 days before the procedure.