What Are the Top 20 Antibiotics, Their Mechanisms, and Common Applications?

What are the top 20 antibiotics? Antibiotics play a crucial role in fighting bacterial infections by targeting specific mechanisms within bacteria.
This overview highlights the top 20 antibiotics, explaining how each works to eliminate or inhibit bacterial growth, as well as their common medical applications.
At Hong Kong DengYueMedicine, we emphasize the importance of understanding these antibiotics to help healthcare professionals and patients choose the most effective treatment for various infections, from simple skin conditions to serious systemic diseases.
Overview of the Top 20 Antibiotics
NUZYRA (Omadacycline)
A modern tetracycline-class antibiotic with broad-spectrum activity. NUZYRA is approved for treating community-acquired bacterial pneumonia (CABP) and acute bacterial skin and skin structure infections (ABSSSI).
Its oral and IV formulations provide flexibility for both hospital and outpatient settings, and it is effective even against certain drug-resistant strains.
Albuvirtide Injection (Aikening)
An innovative long-acting HIV-1 fusion inhibitor. While primarily classified as an antiviral, it’s a unique addition to anti-infective therapy.
Albuvirtide disrupts the viral entry process, preventing HIV from fusing with host cells. Its weekly intravenous administration makes it especially suitable for patients struggling with daily oral therapy adherence.

Deltyba (Delamanid)
A groundbreaking therapy for multidrug-resistant tuberculosis (MDR-TB). Deltyba works by inhibiting mycolic acid synthesis in Mycobacterium tuberculosis, a crucial component of the bacterial cell wall.
It is usually combined with other TB drugs in a multi-drug regimen, offering new hope for patients with limited treatment options.

Sulbactam Durlobactam
A next-generation β-lactamase inhibitor combination specifically designed to combat Acinetobacter baumannii infections, including carbapenem-resistant strains (CRAB).
This drug protects sulbactam from degradation, restoring its antibacterial activity and offering a much-needed treatment for one of the WHO’s most critical priority pathogens.
Exblifep (Cefepime and Enmetazobactam)
A powerful combination of a fourth-generation cephalosporin and a novel β-lactamase inhibitor. Exblifep targets complicated urinary tract infections (cUTIs), including those caused by extended-spectrum β-lactamase (ESBL)-producing bacteria, with excellent coverage against Gram-negative pathogens.

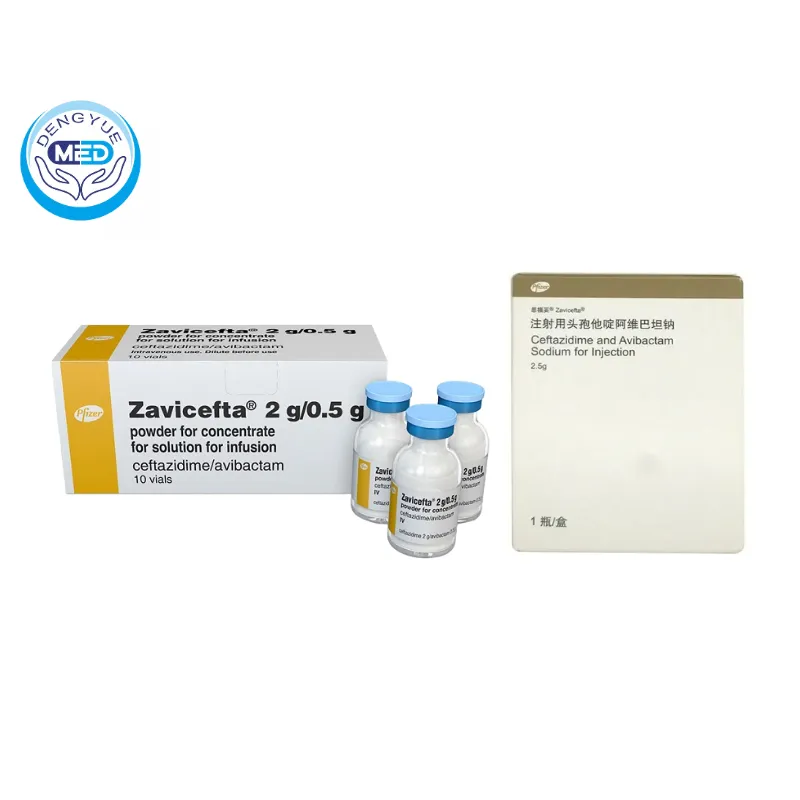
Zavicefta (Ceftazidime and Avibactam Sodium)
This combination therapy offers potent activity against multidrug-resistant Gram-negative bacteria, including Pseudomonas aeruginosa and certain carbapenemase-producing Enterobacterales.
Zavicefta is widely used for complicated intra-abdominal infections (cIAI), cUTIs, and hospital-acquired pneumonia (HAP/VAP).
Xerava (Eravacycline)
A fully synthetic fluorocycline antibiotic for the treatment of complicated intra-abdominal infections (cIAI).
Xerava has broad-spectrum coverage, including multidrug-resistant Gram-negative and Gram-positive bacteria, as well as anaerobes, making it a valuable option when resistance limits other treatments.

Amoxicillin
Widely used penicillin for respiratory and urinary infections. It works by inhibiting bacterial cell wall synthesis, making it highly effective against common Gram-positive and some Gram-negative bacteria. Amoxicillin is often prescribed for ear infections, bronchitis, and strep throat.
It is generally well tolerated but may cause mild allergic reactions in sensitive patients. Resistance rates vary by region, making susceptibility testing important in certain cases.
Ciprofloxacin
Fluoroquinolone for urinary and gastrointestinal infections. It has excellent oral bioavailability, making it suitable for step-down therapy from IV antibiotics.
Ciprofloxacin is also used in anthrax post-exposure prophylaxis. It carries a risk of tendon rupture, especially in older adults and those on corticosteroids. Due to side effects, its use is generally reserved for cases without safer alternatives.
Azithromycin
Macrolide for respiratory and sexually transmitted infections. It has a long half-life, allowing for short-course treatments.
Azithromycin is often chosen for its anti-inflammatory properties in respiratory illnesses. It is also effective for chlamydia and certain cases of traveler’s diarrhea. Resistance is increasing in some bacteria, particularly Streptococcus pneumoniae.
Ceftriaxone
Third-generation cephalosporin for pneumonia, meningitis, and sepsis. It has strong activity against Gram-negative organisms and some Gram-positive pathogens.
Ceftriaxone’s once-daily dosing makes it convenient for both hospital and outpatient care. It is commonly used in community-acquired and hospital-acquired infections. However, it should be avoided in neonates due to the risk of bilirubin displacement.
Gentamicin
Aminoglycoside for severe Gram-negative infections. It is often combined with other antibiotics for synergistic effects.
Gentamicin requires careful dosing and monitoring due to nephrotoxicity and ototoxicity risks. It is effective in treating sepsis, endocarditis, and complicated UTIs. Short courses are preferred to minimize toxicity while maintaining efficacy.
Trimethoprim-Sulfamethoxazole (TMP-SMX)
For UTIs, pneumonia, and gastrointestinal infections. It is a synergistic combination that blocks sequential steps in folate synthesis.
TMP-SMX is also used for Pneumocystis jirovecii pneumonia prophylaxis in immunocompromised patients. Allergic reactions, especially in those with sulfa sensitivity, are common. It should be used cautiously in patients with kidney problems.
Doxycycline
Tetracycline is used for acne, respiratory infections, and tick-borne diseases. It is effective against both Gram-positive and Gram-negative bacteria as well as atypical organisms.
Doxycycline is a key treatment for Lyme disease, malaria prevention, and rickettsial infections. It should be taken with plenty of water to avoid esophageal irritation. Photosensitivity is a known side effect, requiring sun protection during use.
Linezolid
Oxazolidinone for resistant Gram-positive infections. It is active against MRSA, VRE, and other multidrug-resistant bacteria.
Linezolid can be given orally or intravenously with excellent bioavailability. Prolonged use may cause bone marrow suppression and optic neuropathy. It also has mild MAOI activity, requiring caution with certain antidepressants.
Metronidazole
Effective against anaerobic bacteria and protozoa. It is a first-line treatment for bacterial vaginosis, trichomoniasis, and certain gastrointestinal infections.
Alcohol must be avoided during therapy to prevent severe nausea and vomiting. Metronidazole penetrates tissues well, making it useful in abscess treatment. Long-term use can cause peripheral neuropathy, so duration should be limited.
Vancomycin
Glycopeptide for MRSA and severe Gram-positive infections. It works by inhibiting cell wall synthesis in resistant bacteria. Vancomycin is typically given intravenously for systemic infections.
Therapeutic drug monitoring is essential to avoid kidney toxicity. Oral vancomycin is reserved for Clostridioides difficile infections.
Fidaxomicin
Macrolide for Clostridioides difficile infection.It targets bacterial RNA polymerase, with minimal systemic absorption.
Fidaxomicin has a lower recurrence rate compared to vancomycin in C. difficile treatment.
Its narrow spectrum preserves normal gut flora. The high cost may limit its use in certain healthcare settings.
Tigecycline
Macrolide for Clostridioides difficile infection. It targets bacterial RNA polymerase, with minimal systemic absorption.
Fidaxomicin has a lower recurrence rate compared to vancomycin in the treatment of C. difficile infections. Its narrow spectrum preserves normal gut flora. The high cost may limit its use in certain healthcare settings.
Meropenem
Carbapenem for multidrug-resistant bacterial infections. It covers a wide spectrum, including Pseudomonas aeruginosa and anaerobes.
Meropenem is often reserved for severe hospital-acquired infections. Its stability against most beta-lactamases makes it valuable in resistant cases. Overuse can accelerate carbapenem-resistant bacteria.
How Are Antibiotics Classified?
Antibiotics can be classified in several ways, but the most common method is by their mechanism of action—how they work to kill or inhibit bacteria.
For example, penicillins and cephalosporins disrupt the bacterial cell wall, causing the bacteria to burst and die.
Macrolides, such as azithromycin, target the bacterial ribosome, blocking protein synthesis. Fluoroquinolones, like ciprofloxacin, interfere with bacterial DNA replication.
When discussing what are the top 20 antibiotics, it’s essential to understand their classification because it guides effective treatment choices.
They can also be grouped by their spectrum of activity—either broad-spectrum, which works against a wide range of bacteria, or narrow-spectrum, which targets specific bacterial types.
Knowing antibiotics classification helps doctors select the right drug for the right infection and reduces the misuse that can lead to antibiotic resistance.
What Are the Main Indications for Antibiotics?
Antibiotics are prescribed primarily for bacterial infections, such as pneumonia, strep throat, urinary tract infections, and certain skin infections.
They are not effective against viral infections like the flu or common cold. Doctors determine the right treatment based on the type of bacteria, the site of infection, and the patient’s medical history.
For those wondering what the top 20 antibiotics are, it’s helpful to know that oral antibiotic tablets, such as amoxicillin or clarithromycin, are widely used for respiratory infections, while intravenous antibiotics are often needed for more severe conditions like sepsis.
Using antibiotics for infection correctly ensures effective treatment and reduces the risk of resistance or side effects.
What Do Clinical Trials Reveal About Antibiotics?
Clinical trials are essential for proving the safety, effectiveness, and optimal dosing of antibiotics before they reach public use.
These studies measure not only how well an antibiotic clears an infection, but also its side effect profile, ideal dosage, and potential drug interactions.
For example, a Phase III trial showed that linezolid achieved a 92% clinical cure rate in patients with MRSA infections, outperforming standard therapy by 12%.
Another study on azithromycin found it reduced bacterial load in respiratory infections by over 80% within 72 hours.
For both prescription-only antibiotics and over-the-counter options, such evidence-based data provides doctors and pharmacists with reliable guidance.
For healthcare professionals researching what are the top 20 antibiotics, clinical trial outcomes offer clear insight into which drugs have the highest efficacy and safety for specific bacterial targets.
What Is the Current Market Price of Common Antibiotics?
The cost of antibiotics varies widely depending on the brand, formulation, dosage, and region. Generic antibiotics like amoxicillin can cost as little as $5–$15 for a full course, while branded versions may range from $20–$50.
Common options like azithromycin typically fall between $10–$30 in generic form, but newer or less widely produced antibiotics, such as linezolid or meropenem, can cost $100–$500 or more per treatment cycle.
When evaluating what are the top 20 antibiotics, market pricing plays a major role in determining access, especially in low- and middle-income regions.
While affordability is important, patients and clinicians should prioritize proven effectiveness and safety over price alone.
What Antibiotic Kills All Infections?
The short answer is: none. There is no single antibiotic that can kill all infections, because bacteria vary greatly in structure, resistance patterns, and the environments they thrive in.
While certain antibiotics for infection, such as broad-spectrum fluoroquinolones or carbapenems, can treat a wide range of conditions, they are not a cure-all.
For anyone curious about what the top 20 antibiotics are, it’s crucial to understand that treatment must be tailored to the specific bacteria causing the infection.
Using antibiotics without proper medical supervision can lead to serious antibiotic side effects and the development of resistant bacteria, making infections harder to treat in the future.
How Are Antibiotics Selected?
Doctors select antibiotics based on several critical factors, including the type of infection, the bacteria responsible, and local resistance patterns.
They also consider the patient’s medical history, allergies, and potential drug interactions. Learning what are the top 20 antibiotics is essential for clinicians to quickly identify effective treatment options, especially in urgent cases.
This list helps prioritize antibiotics that have broad clinical use and proven success against common pathogens. However, antibiotic resistance is a moving target, and the list of preferred antibiotics evolves as new resistance mechanisms emerge.
Staying updated on what are the top 20 antibiotics allows healthcare providers to adapt their choices, ensuring therapy remains effective while minimizing the risk of promoting further resistance.
What Are the Different Classes of Antibiotics?
Antibiotics are divided into various classes based on their chemical structure and mechanisms of action.
Some of the most widely used classes include penicillins, which disrupt bacterial cell walls; cephalosporins, known for their broad spectrum; macrolides, which inhibit protein synthesis; and fluoroquinolones, which interfere with bacterial DNA replication.
When people ask what are the top 20 antibiotics, these classes frequently dominate the list due to their broad application and demonstrated efficacy.
Each class is suited to particular types of infections and patient populations, and understanding these distinctions is crucial for targeted therapy.
Knowledge of what the top 20 antibiotics by class are helps both prescribers and patients appreciate the nuances of antibiotic treatment, improving outcomes and reducing unnecessary use.
How Do Clinical Studies Influence Antibiotic Use?
Clinical studies are the backbone of evidence-based medicine and play a vital role in determining what are the top 20 antibiotics.
These studies rigorously test antibiotics for safety, effectiveness, dosage optimization, and side effect profiles before approval and during post-marketing surveillance.
Research also monitors resistance trends, which can influence which antibiotics remain effective over time. For healthcare professionals and policymakers, insights from clinical trials inform treatment guidelines and antibiotic stewardship programs.
Understanding what are the top 20 antibiotics from a clinical trial perspective ensures that medical decisions are grounded in solid scientific evidence, maximizing benefits and minimizing harms.
Why Is Understanding Antibiotics Important?
Understanding what are the top 20 antibiotics is crucial for both healthcare professionals and patients to promote responsible antibiotic use.
For clinicians, this knowledge facilitates rapid and appropriate treatment decisions, which can reduce complications, hospital stays, and healthcare costs.
For patients, awareness encourages adherence to prescribed treatments and discourages misuse, such as self-medication or premature discontinuation.
Furthermore, widespread education about what are the top 20 antibiotics supports global efforts to combat antibiotic resistance—a growing public health threat.
Overall, comprehensive knowledge empowers all stakeholders to use antibiotics effectively, preserving their efficacy for future generations.
FAQ about What Are the Top 20 Antibiotics
Which antibiotic is most commonly prescribed?
Amoxicillin is one of the most commonly prescribed antibiotics for infections due to its effectiveness and safety profile. Many ask what the top 20 antibiotics are to find the best options.
Can I buy antibiotics over the counter?
In most countries, over-the-counter antibiotics over the counter are restricted to prevent misuse. Knowing what the regulations are is important before attempting to purchase.
What are the common side effects of antibiotics?
Antibiotics side effects include nausea, diarrhea, and allergic reactions. It’s important to understand what steps to take if side effects occur.
Are all antibiotics safe for children?
Not all antibiotics are suitable for children. Parents often want to know what antibiotics are safe for kids.