Colorectal Cancer Causes: 4 Key Risk Factors You Should Know
Colorectal cancer is one of the most common and serious types of cancer worldwide, affecting both the colon and rectum.
Understanding colorectal cancer causes is essential for prevention, early detection, and effective treatment.
Key contributing factors include genetic predisposition, chronic inflammatory bowel diseases, unhealthy dietary habits, obesity, sedentary lifestyle, smoking, and excessive alcohol consumption.
Research and clinical studies consistently highlight how these factors interact to increase the risk of developing colorectal cancer, emphasizing the importance of awareness and proactive health measures.
At Hong Kong DengYue Medicine, we emphasize the importance of understanding these warning signs to help healthcare professionals and patients detect cervical cancer early and select the most effective treatments.
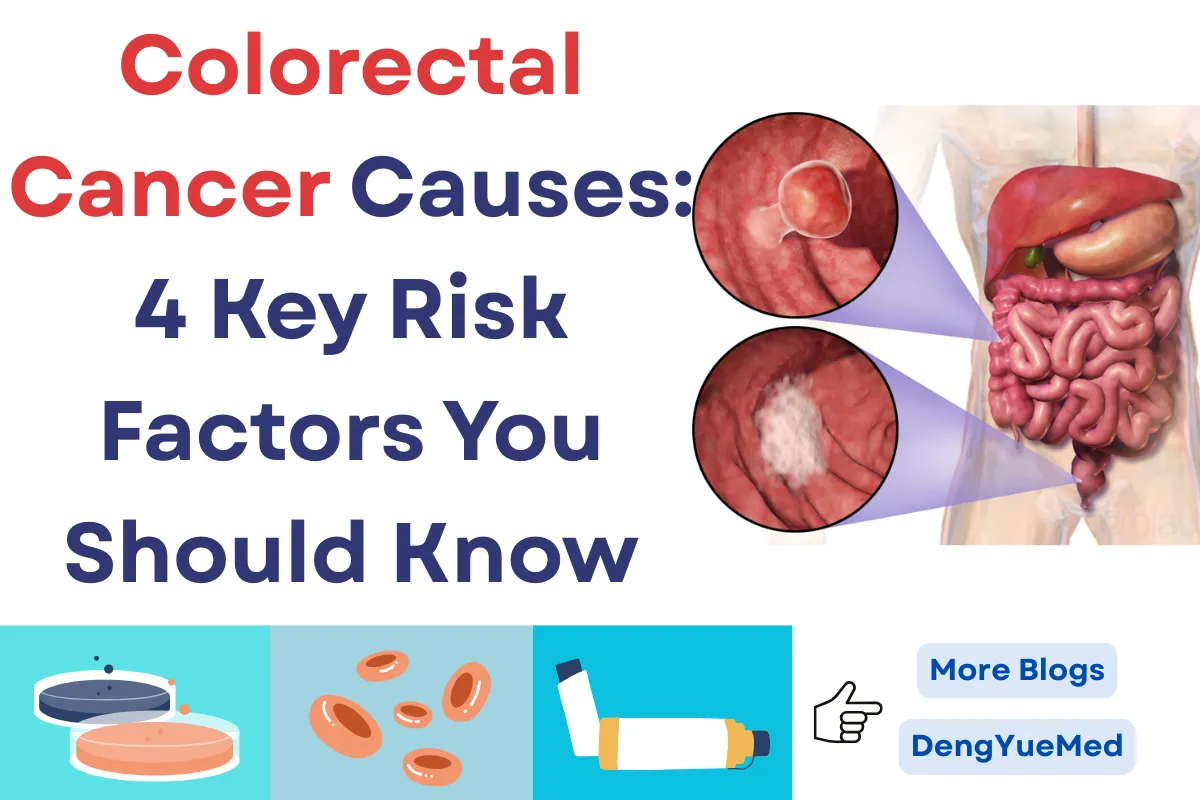
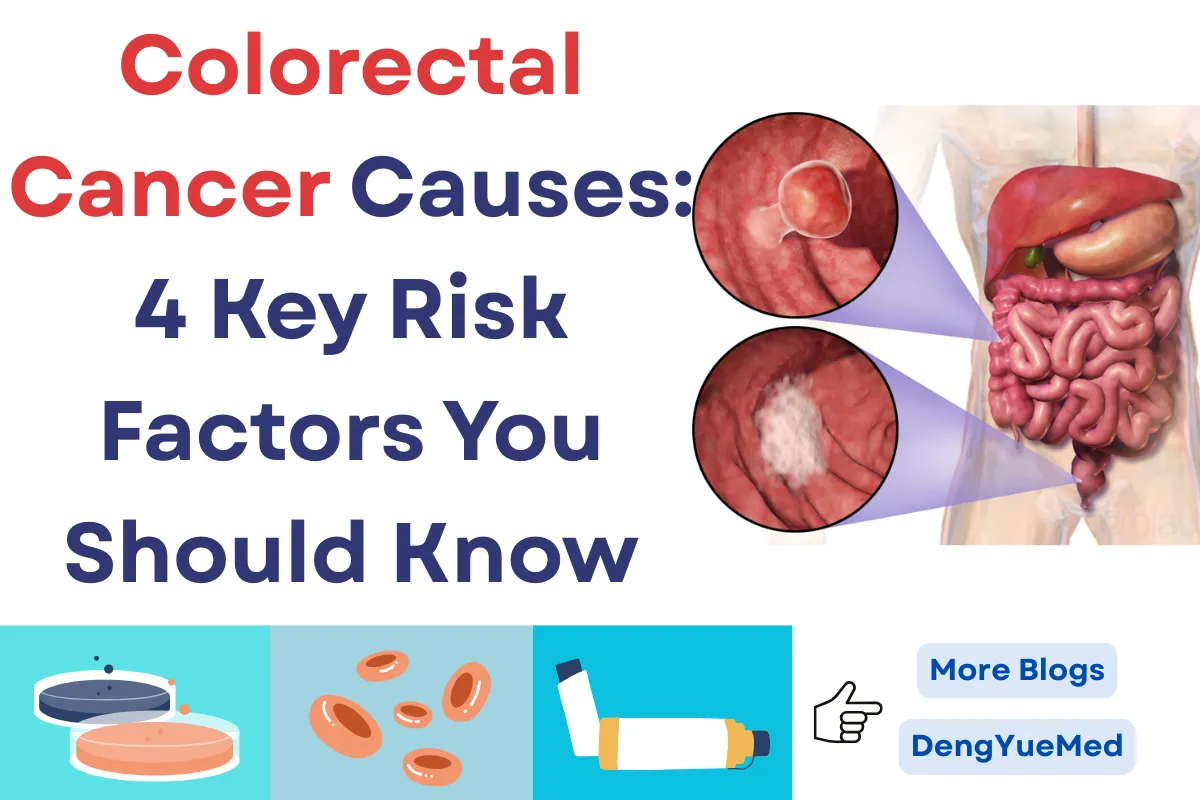
What Is The Definition Of Colorectal Cancer?
Colorectal cancer (CRC) is a type of malignancy that originates in the colon or rectum, making it one of the most common cancers worldwide.
Most colorectal cancers begin as adenomatous polyps, which can develop into malignant tumors over several years.
Epidemiological studies show that approximately 1 in 23 men and 1 in 25 women will be diagnosed with colorectal cancer during their lifetime.
Understanding colorectal cancer causes is crucial for early detection and prevention, as both genetic predispositions and environmental or lifestyle factors play significant roles in tumor development.
Who Is At High Risk For Colon Cancer?
High-risk individuals include those with a family history of colorectal cancer, inherited genetic syndromes like Lynch syndrome or familial adenomatous polyposis (FAP), and chronic inflammatory bowel diseases such as ulcerative colitis or Crohn’s disease.
Clinical studies indicate that people with FAP have nearly a 100% lifetime risk of developing colorectal cancer if untreated.
Lifestyle factors, such as smoking, obesity, excessive alcohol consumption, and diets high in red or processed meats, also significantly contribute to colorectal cancer causes. Research shows these modifiable factors can increase colorectal cancer risk by 40–50%.
At What Age Do People Get Colon Cancer?
Colorectal cancer incidence increases with age, with most cases diagnosed after age 50.
However, recent epidemiological data reveal a growing trend of early-onset CRC in individuals under 50, accounting for 10–15% of new cases in the United States.
The rise is linked to lifestyle-related colorectal cancer causes, such as poor diet, obesity, sedentary behavior, and metabolic syndrome.
Early screening starting at age 45 is now recommended to detect precancerous lesions in younger adults.
What Is The Biggest Symptom Of Colon Cancer?
The biggest and most common symptom of colon cancer is rectal bleeding or blood in the stool. This occurs because tumors in the colon or rectum damage the intestinal lining, leading to visible or hidden bleeding.
Studies show that nearly 50% of patients report bleeding as their first noticeable sign. Since this symptom can also be mistaken for hemorrhoids, it is often ignored, causing delays in diagnosis.
If you notice persistent rectal bleeding, even in small amounts, it is crucial to seek medical evaluation immediately, as early detection greatly improves treatment outcomes.
🌟 Don’t ignore the signs—taking action early could save your life! 💪
What Are the 4 Key Risk Factors of Colorectal Cancer’s Causes?
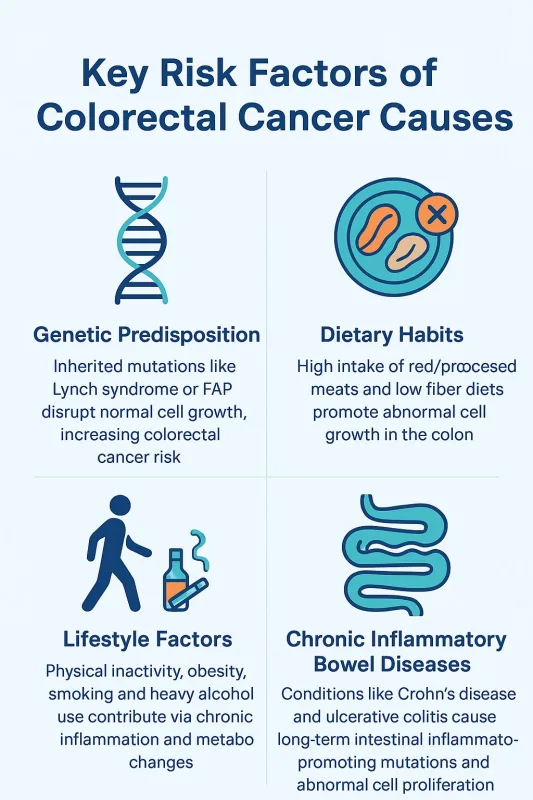
Genetic Predisposition
Inherited genetic mutations, such as those seen in Lynch syndrome or familial adenomatous polyposis (FAP), significantly increase the risk of developing colorectal cancer.
Individuals with a family history of colorectal cancer have a 2–3 times higher risk than those without. These mutations disrupt normal cell growth and repair mechanisms, leading to uncontrolled cell proliferation.
Clinical studies indicate that FAP patients who do not undergo preventive colectomy have nearly a 100% lifetime risk of developing colorectal cancer.
Genetic counseling and regular colonoscopy screenings are strongly recommended for high-risk individuals to monitor and reduce the risk associated with these colorectal cancer causes.
Dietary Habits
Diet is one of the most significant modifiable colorectal cancer causes. High intake of red and processed meats, combined with low fiber consumption, is strongly linked to increased colorectal cancer risk.
Studies show that individuals consuming more than 100 grams of red or processed meat daily have a 20–30% higher risk of colorectal cancer.
Diets rich in fruits, vegetables, whole grains, and legumes can reduce risk by providing antioxidants, vitamins, and fiber that promote healthy bowel function and reduce inflammation.
Public health guidelines recommend limiting red meat and processed meat consumption and increasing dietary fiber to counteract diet-related colorectal cancer causes.
Lifestyle Factors
Lifestyle choices are critical contributors to colorectal cancer. Physical inactivity and obesity can lead to insulin resistance, chronic inflammation, and metabolic syndrome, all of which promote tumor development.
Smoking introduces carcinogens that directly damage DNA in colon cells, while heavy alcohol consumption alters gut microbiota and increases acetaldehyde exposure, a known carcinogen.
Data from large cohort studies indicate that maintaining a healthy weight, engaging in regular physical activity, avoiding tobacco, and limiting alcohol consumption can reduce colorectal cancer risk by 30–40%.
These findings highlight the importance of lifestyle modification in preventing these key colorectal cancer causes.
Chronic Inflammatory Bowel Diseases
Chronic inflammation of the intestinal lining is a well-documented factor in colorectal cancer causes. Conditions such as Crohn’s disease and ulcerative colitis cause repeated cycles of inflammation and healing, which can lead to DNA damage and increase the risk of cancer development over time.
Long-term studies show that patients with ulcerative colitis for more than 8–10 years have a significantly higher risk of colorectal cancer, with risk increasing further with disease severity and extent.
Regular surveillance colonoscopies, anti-inflammatory treatment, and careful disease management are recommended strategies to mitigate the impact of chronic inflammatory conditions on colorectal cancer risk.
Cervical Cancer Treatments: Key Therapies You Should Know
For patients exploring colorectal cancer treatment, the following seven therapies are commonly used and offer effective options for management.
Azathioprine Tablets

Primarily used as an immunosuppressant, azathioprine can be applied as supportive therapy in patients with inflammatory bowel diseases that predispose them to colorectal cancer.
Controlling chronic inflammation reduces the risk of malignant transformation and helps maintain long-term remission.
Compound Fluorouracil Oral Solution

This oral formulation of 5-fluorouracil is widely applied in gastrointestinal malignancies, especially advanced colorectal cancer.
Compound fluorouracil oral solution allows for continuous exposure to the drug, offering effective tumor suppression with greater convenience compared to intravenous infusion.
Carmofur Tablets
Carmofur, a derivative of 5-fluorouracil, is an oral chemotherapeutic agent used in colorectal cancer management.
Its convenient dosing makes it suitable for long-term therapy, and it has shown efficacy in controlling tumor progression in clinical practice.
Garsorasib
As a novel KRAS G12C inhibitor, Garsorasib represents a breakthrough for patients with mutation-driven solid tumors, including subsets of colorectal cancer.
Early clinical studies highlight its potential to selectively target cancer-driving mutations with precision.
Fruquintinib Capsules

Fruquintinib is a highly selective VEGFR inhibitor approved for metastatic colorectal cancer. Clinical trials, such as the FRESCO study, demonstrated significant improvements in progression-free survival and overall survival, establishing it as an important targeted therapy option.
Lonsurf (Trifluridine/Tipiracil)

This oral chemotherapy combination is indicated for metastatic colorectal cancer patients who have progressed after standard therapies.
Clinical evidence shows that Lonsurf prolongs survival and offers manageable toxicity, making it a vital option in late-line treatment.
YERVOY (Ipilimumab)
As a CTLA-4 immune checkpoint inhibitor, Yervoy enhances T-cell activation and immune response against cancer.
In colorectal cancer, it has demonstrated efficacy when combined with PD-1 inhibitors, especially in microsatellite instability-high (MSI-H) or mismatch repair-deficient (dMMR) tumors.
How Long Can You Have Colon Cancer Without Knowing?
Colon cancer usually develops slowly and can remain unnoticed for many years. The progression often follows these stages:
- 0–3 years: Small benign polyps form in the colon lining. Studies show that over 25% of adults above 50 may have polyps, but most experience no symptoms.
- 3–7 years: Polyps gradually enlarge, and some develop precancerous changes. According to the National Cancer Institute, the adenoma-to-carcinoma sequence typically takes at least 5 years.
- 7–10 years: Certain polyps transform into malignant tumors. Data from long-term cohort studies suggest that it usually takes 7–10 years for adenomatous polyps to progress to invasive colorectal cancer.
- 10+ years: Once cancer advances, symptoms like rectal bleeding, unexplained anemia, abdominal pain, or changes in bowel habits may appear. By this stage, many cases are diagnosed at a later stage.
This timeline indicates that colon cancer can remain silent for 7–10 years or more. The American Cancer Society emphasizes that regular colonoscopy every 10 years (or sooner for high-risk individuals) can detect and remove polyps early, preventing up to 76–90% of colorectal cancers.
✨ Remember: early screening saves lives—take action for your health today! 💙
Is Colorectal Cancer Curable?
Yes, colorectal cancer can be curable, especially when detected at an early stage. Treatment typically involves a combination of medical approaches tailored to the stage and overall health of the patient:
- Surgery: The primary treatment for early-stage colorectal cancer. Removing the tumor and surrounding tissue can completely eliminate the disease in many patients.
- Chemotherapy: Often used after surgery (adjuvant therapy) to kill remaining cancer cells or in advanced stages to control tumor growth. Drugs such as fluorouracil (5-FU), oxaliplatin, and capecitabine are widely used.
- Radiation Therapy: Particularly effective for rectal cancer, often given before surgery to shrink tumors and reduce recurrence risk.
- Targeted Therapy & Immunotherapy: Medications like bevacizumab, cetuximab, and immunotherapies such as PD-1 inhibitors help attack cancer cells more precisely, offering hope in advanced stages.
- Clinical Trials: Ongoing studies provide access to cutting-edge treatments, improving survival and quality of life.
Survival outcomes strongly depend on the stage at diagnosis. According to the American Cancer Society, the 5-year survival rate is over 90% for stage I, but only about 14% for stage IV. This highlights the life-saving importance of early screening and prompt treatment.
💙 With early detection and modern therapies, there is real hope—never lose courage, because every step forward brings you closer to recovery! 🌟
What Is The Life Expectancy Of A Person With Colon Cancer?
Life expectancy varies based on cancer stage, overall health, and response to treatment. Early detection through screening increases survival rates dramatically.
For localized colorectal cancer, the 5-year survival rate is nearly 90%, while advanced metastatic cases have a much lower survival rate.
Addressing modifiable colorectal cancer causes, including diet, exercise, and regular screening, can improve outcomes and reduce mortality.
Clinical evidence from large cohort studies emphasizes that preventive strategies targeting these causes are highly effective in reducing disease burden.
FAQ about Colorectal Cancer Causes: 4 Key Risk Factors You Should Know
What Is The Main Cause Of Colorectal Cancer?
Colorectal cancer usually develops when genetic mutations accumulate in the cells of the colon or rectum.
These mutations disrupt normal cell growth and division, allowing abnormal cells to multiply uncontrollably and form tumors.
Both inherited genetic factors and acquired mutations over a person’s lifetime can contribute.
What Lifestyle Leads To Colon Cancer?
Certain lifestyle factors increase the risk of developing colon cancer. A diet high in red and processed meats, low in fiber, excessive alcohol consumption, smoking, physical inactivity, and obesity are all linked to a higher risk.
Long-term exposure to these factors can lead to changes in colon cells that may eventually develop into cancerous cells.
Can Colon Cancer Be Cured Permanently?
Colon cancer can often be cured if detected early, especially through surgical removal of tumors and, in some cases, additional treatments like chemotherapy or radiation.
However, advanced or metastatic colorectal cancer may require long-term management, and regular follow-up is essential to monitor for recurrence.
Who Is Most Likely To Get Colon Cancer?
Colon cancer is more common in people over the age of 50, but younger individuals with a family history or certain genetic syndromes are also at risk.
Lifestyle factors such as poor diet, lack of exercise, obesity, smoking, and heavy alcohol use further increase susceptibility.
People with a history of inflammatory bowel disease, such as ulcerative colitis or Crohn’s disease, are also at higher risk.