New COPD Treatment Launched: What’s New in 2025 and What’s Next for Global and China COPD Care
🫁 Chronic Obstructive Pulmonary Disease (COPD) is a progressive respiratory condition characterized by persistent airflow limitation and chronic airway inflammation.
🤔 Today, COPD remains a major global health challenge and continues to place a growing burden on healthcare systems worldwide.
According to the Global Burden of Disease (GBD) and the World Health Organization (WHO), global estimates suggest that more than 300–390 million people worldwide are currently living with COPD, making it one of the most prevalent chronic respiratory diseases.
The disease has become the third leading cause of death globally, responsible for over 3 million deaths each year.
Its prevalence continues to rise due to aging populations, sustained smoking exposure, and worsening air quality.
In China, the burden is equally significant, with an adult prevalence close to 8%, affecting tens of millions of individuals and representing a major public health challenge.
👉 Against this backdrop of rising prevalence and limited disease control, the new COPD treatment launched in 2025 marks a critical turning point rather than a routine incremental update.
✨ Recent advances, including nebulized triple therapy, biologics, dual-pathway small-molecule agents, and phenotype-specific precision treatments, represent a major step forward in reducing exacerbations, improving lung function, and enhancing patient quality of life.
In the following sections, DengYueMed will guide you through a clear overview of COPD’s causes and symptoms and provide an in-depth explanation of the latest COPD therapies launched in 2025, offering an up-to-date perspective on how this disease is being managed globally and in China.
What are The Breakthroughs for COPD in 2025?
Chronic obstructive pulmonary disease (COPD) is a progressive respiratory disorder characterized by persistent airflow limitation and chronic inflammation of the airways.
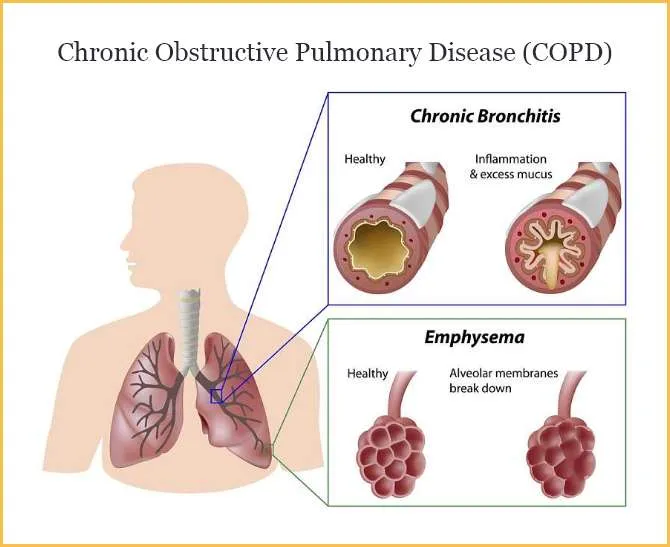
🚬 It is primarily caused by long-term exposure to harmful particles or gases—most commonly cigarette smoke.
🌿 Additional contributors include air pollution, biomass fuel exposure, and occupational dust or chemical exposure, particularly in developing regions.
Patients typically experience chronic cough, sputum production, dyspnea, and recurrent exacerbations that worsen lung function over time.
☹️ Despite the availability of standard COPD treatment medications, many individuals still face uncontrolled symptoms, frequent flare-ups, or progressive decline.
✨ For these reasons, 2025 became a pivotal moment, marked by multiple new COPD treatment launched announcements and the introduction of new treatments for COPD that offer more mechanism-specific action.
These innovations aim to simplify use for certain patient groups while targeting both airway mechanics and underlying inflammatory pathways.
A New Era of Mechanism-Driven Innovation
The year 2025 marks a turning point in COPD therapy, with multiple breakthroughs that move beyond traditional bronchodilation and inhaled corticosteroids.
Instead of relying solely on airflow improvement, the latest therapeutic advances target both airway obstruction and underlying inflammation, offering more comprehensive disease control.
✅ These new mechanisms are supported by improved biomarker understanding, patient phenotyping, and advancements in inhalation and injection-based delivery technologies.
What is the newest treatment for COPD? There are:
1. Dual-Pathway Mechanisms Become the New Standard
One of the most important trends in 2025 is the rise of dual-pathway therapies, designed to address the two central drivers of COPD progression:
- Airway smooth-muscle constriction (bronchoconstriction)
- Chronic airway inflammation
Unlike conventional single-target drugs, these new therapies modulate two biological pathways at the same time, leading to stronger and more sustained improvements.
The most representative innovation is the development of PDE3/4 dual inhibitors, which combine:
- PDE3 inhibition → bronchodilation, improving lung function
- PDE4 inhibition → anti-inflammatory effect, reducing cytokine release and exacerbation risk
✅ This dual mechanism provides benefits comparable to combining several inhaled therapies but in a single molecule with a more stable pharmacodynamic profile.
2. Enhanced Bronchodilation Through Dual-Action Targets
Several 2025 candidates also explore bronchodilation through simultaneous activation or inhibition of multiple smooth-muscle signaling pathways, such as:
- β2-receptor agonism + muscarinic receptor modulation
- Novel ion-channel targets regulating airway tone
- Long-acting modulators of airway hyperresponsiveness
✅ These therapies deliver stronger and longer-lasting airway relaxation while reducing the need for frequent inhalations—particularly useful for elderly patients.
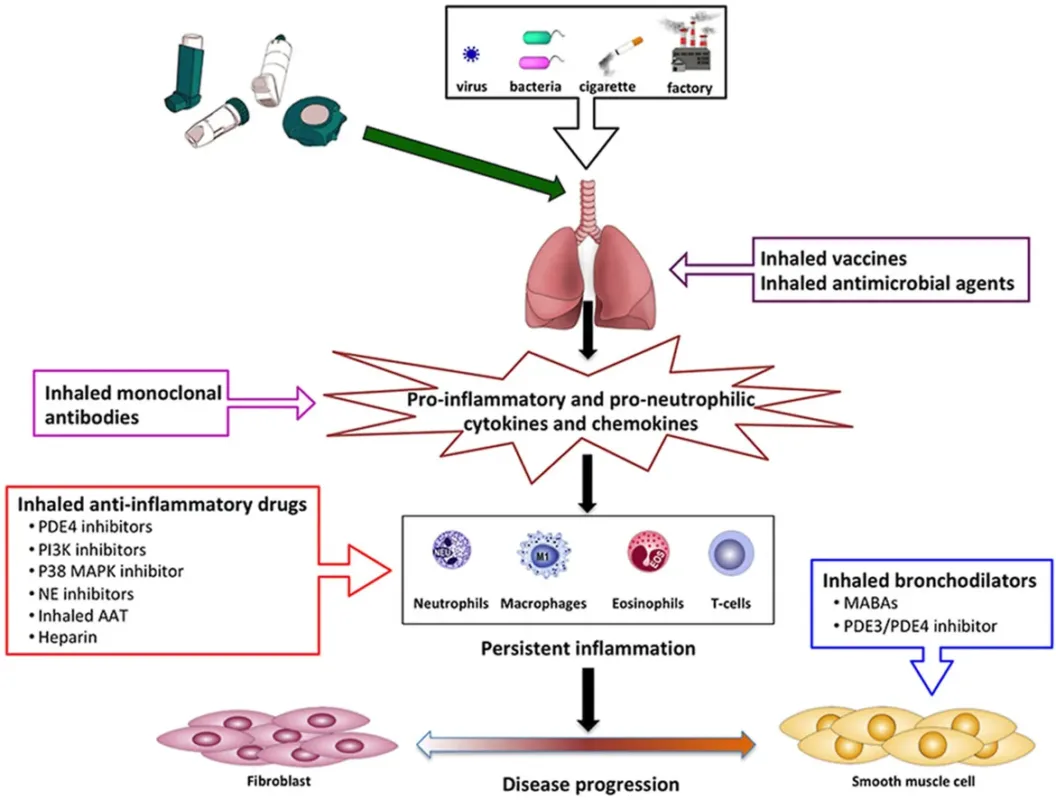
3. Anti-Inflammatory Innovation Beyond Traditional Steroids
Inflammation-targeting therapies in 2025 are no longer limited to inhaled corticosteroids (ICS). This year’s pipeline introduces:
- Selective cytokine inhibitors
- Inhaled anti-inflammatory small molecules
- Systemic biologics acting on Type 2 inflammation and eosinophilic pathways
- Molecules controlling oxidative stress and neutrophil activation
✅ These approaches focus on the deeper immunological mechanisms that drive frequent exacerbations and long-term disease progression—significantly improving outcomes for patients who previously responded poorly to ICS.
4. Synergistic Designs for Exacerbation Prevention
A major focus of the 2025 innovations is preventing acute exacerbations, which are the biggest contributor to COPD mortality and healthcare burden. New dual-pathway and multi-target drugs demonstrate:
- Fewer flare-ups
- Improved daily symptom control
- Better quality of life
- Reduced need for rescue medication
✨ This shift from reactive treatment to proactive disease suppression is one of the defining breakthroughs of 2025.
The breakthroughs of 2025 show a clear pattern:COPD therapy is shifting from simple bronchodilation to mechanism-driven, dual-pathway, and multi-target solutions.
By integrating bronchodilation with advanced anti-inflammatory strategies, these innovations are redefining what effective COPD management looks like.
What is The Latest Drug for COPD?
In 2025, COPD treatment has expanded beyond traditional inhaler-based therapy, reflecting the industry’s shift toward mechanism-specific and inflammation-targeting interventions.
While bronchodilators and inhaled corticosteroids remain core components of standard care, the latest COPD treatment options now include dual-pathway bronchodilation, advanced anti-inflammatory agents, biologics, and novel non-inhaler delivery systems.
These developments provide alternatives for patients who are unable to use inhalers correctly, have persistent symptoms, or experience treatment-resistant disease phenotypes.
Several next-generation COPD therapies launched in 2025 are designed to address both airflow limitation and underlying airway inflammation.
New drug classes focus on modulating neutrophilic inflammation, inhibiting epithelial-derived cytokines, improving mucociliary function, or reducing airway remodeling.
In parallel, digital-health-supported drug–device combinations and systemic formulations are improving accessibility and adherence for broader patient groups.
👉 Together, these innovation trends reflect a move toward personalized COPD therapy—matching mechanisms to patient phenotypes and offering more effective, convenient, and biologically targeted treatment options than ever before.
New COPD Treatment Injection
Among the most notable advances in 2025 is the introduction of new COPD treatment injections, marking a significant shift away from inhaler-only management.
These injectable therapies are designed to provide longer-lasting airway control, reduce exacerbation rates, and target inflammatory drivers that inhalers cannot adequately reach.
New injections fall primarily into two categories:
1. Long-acting biologics
These agents target key inflammatory pathways—such as IL-33, TSLP, or neutrophil-driven cascades—to reduce exacerbations in patients with persistent inflammation, chronic bronchitis phenotypes, or frequent flare-ups.
Administered subcutaneously every few weeks or monthly, they provide sustained systemic activity beyond the reach of inhaled drugs.
2. Extended-release bronchodilator injections
Developed for patients with difficulty mastering inhaler technique, these injections help maintain stable bronchodilation over prolonged periods.
Some formulations are being explored as once-monthly maintenance therapy, offering improved adherence and more consistent symptom control.
As part of the broader wave of New COPD treatment launched announcements in 2025, these injectable options offer new flexibility in designing treatment plans.
As more new COPD treatment injections enter global markets, they are expected to play a central role in bridging current therapeutic gaps, supporting personalized treatment pathways, and driving the transition toward mechanism-guided COPD care.
Together, these injectable therapies represent one of the most meaningful advancements in the evolving portfolio of COPD treatment options in 2025.
These innovations are also reshaping how clinicians think about long-term control of chronic obstructive pulmonary disease (COPD)—shifting the focus from daily symptom management to proactively altering the disease trajectory itself.
As these innovations move from clinical trials into real-world practice, they raise a critical question for both patients and healthcare providers: among so many new options, what is currently the most effective approach?
What is The Most Effective Treatment for COPD?
Determining the “most effective” treatment for COPD in 2025 requires acknowledging that no single therapy works for every patient.
🦠 COPD is a heterogeneous condition, influenced by diverse phenotypes, inflammatory pathways, comorbidities, and progression patterns.
As a result, the best therapeutic approach is one that aligns with an individual patient’s biological drivers and clinical needs—a principle that has increasingly shaped modern COPD care.
1. Dual-Pathway Bronchodilators: Foundational for Symptom Control
Long-acting bronchodilators, particularly LABA/LAMA dual therapy, remain the cornerstone of COPD management for improving airflow, reducing daily symptoms, and enhancing exercise tolerance.
In 2025, next-generation dual bronchodilators with improved receptor selectivity and longer duration provide more stable airway relaxation and better exacerbation prevention.
2. Inhaled Triple Therapy for High-Risk Patients
For individuals with frequent flare-ups or elevated eosinophils, inhaled triple therapy (LABA + LAMA + ICS) continues to demonstrate strong clinical effectiveness.
Its ability to modulate airway tone and address eosinophilic inflammation makes it one of the most proven strategies for reducing exacerbations.
3. New Anti-Inflammatory Agents and Biologics
With the launch of multiple new COPD treatment medications in 2025—including biologics targeting IL-33, TSLP, and neutrophil-driven pathways—systemic anti-inflammatory therapy has become a frontrunner for patients with chronic bronchitis phenotypes or persistent inflammation despite inhalers.
For select groups, these agents may represent the most effective modern approach for reducing exacerbations and slowing disease progression.
4. New COPD Treatment Injection Options
The emergence of long-acting injectable bronchodilators and biologics provides an alternative for patients unable to master inhaler technique or those who require sustained, systemic control.
In many cases, these injections outperform conventional therapy in adherence, consistency, and reduction of flare-ups.
5. Pulmonary Rehabilitation and Lifestyle Interventions
Beyond pharmacologic therapy, pulmonary rehabilitation remains one of the most effective interventions across all disease stages.
It improves functional capacity, reduces hospitalization, and enhances quality of life—often more significantly than medication alone. Smoking cessation, vaccination, and physical activity remain foundational to long-term outcomes.
6. Phenotype-Driven, Personalized Treatment
The most effective COPD treatment in 2025 is increasingly personalized.
😷 Patients with eosinophilic inflammation benefit from steroid-responsive therapies; chronic bronchitis phenotypes respond better to anti-inflammatory biologics or mucus-targeting drugs; and emphysema-dominant individuals may require lung-volume–targeted interventions.
Precision medicine is transforming COPD from a uniform treatment model into one tailored to individual disease biology.
❓ As treatment becomes increasingly individualized, the next major question emerges: can COPD eventually be cured?
The following section explores cutting-edge research—from regenerative therapies to gene-targeted strategies—that is redefining what the future of COPD care may look like.
COPD Cure Research—Is A Cure Possible?
While current COPD therapies focus on symptom control, exacerbation reduction, and slowing disease progression, a true cure remains elusive.
COPD involves irreversible structural changes in the lungs, including airway remodeling, alveolar destruction, and chronic inflammation.
Nevertheless, recent advances in regenerative medicine and gene-targeted approaches have sparked optimism for future curative strategies.
1. Regenerative Therapies
Regenerative medicine aims to restore damaged lung tissue and repair alveolar structures. Key approaches under investigation include:
- Mesenchymal stem cells (MSCs): These cells have anti-inflammatory and tissue-repair properties and are being tested in clinical trials to reduce inflammation and promote lung regeneration.
- Induced pluripotent stem cells (iPSCs): iPSCs offer the potential to generate patient-specific lung cells, enabling personalized tissue repair strategies.
- Exosome-based therapies: Derived from stem cells, exosomes can modulate immune responses and promote tissue repair without introducing whole cells.
Early results show promise in reducing inflammation, improving lung function metrics, and potentially slowing structural deterioration, though widespread clinical application is still several years away.
2. Gene-Targeted Approaches
COPD is influenced by multiple genetic and epigenetic factors. Gene-targeted therapies aim to modulate these underlying mechanisms:
- Gene silencing and editing: Targeting specific genes involved in inflammation, protease imbalance, or tissue remodeling could halt disease progression at the molecular level.
- Epigenetic modulators: Drugs that adjust DNA methylation or histone modification patterns may restore healthy gene expression in airway cells.
- Precision biologics: Antibodies and small molecules designed based on patient-specific genetic and phenotypic profiles allow for highly individualized interventions.
Although these strategies are mostly in preclinical or early clinical stages, they represent a paradigm shift: treating the root cause rather than only controlling symptoms.
3. Integrating Regenerative and Targeted Strategies
Future COPD therapy may combine regenerative approaches with phenotype-guided biologics or gene-targeted drugs, offering a multi-pronged strategy:
- Repair damaged alveoli and airways
- Reduce chronic inflammation
- Prevent recurrent exacerbations
- Potentially reverse disease progression in early or moderate stages
These innovations are still experimental, but they lay the groundwork for a long-term vision of a COPD cure.
As research progresses toward curative interventions, understanding disease progression and staging remains critical.
The next section explores the four stages of COPD, helping patients and clinicians select appropriate therapies aligned with disease severity and risk profile.
What are The Four Stages of COPD?
COPD progression is commonly classified into four stages according to the GOLD (Global Initiative for Chronic Obstructive Lung Disease) criteria.
Understanding these stages helps clinicians tailor treatment plans and empowers patients to engage in proactive disease management.
1. Stage 1 — Mild COPD (GOLD 1)
- Characteristics: FEV1 ≥ 80% predicted. Often few or mild symptoms.
- Common Symptoms: Occasional cough, sputum production, and mild shortness of breath during intense activity.
- Treatment Approach:
- Short-acting bronchodilators (SABA or short-acting muscarinic antagonists) as needed
- Lifestyle interventions, including smoking cessation and vaccination
- Patient education to recognize early symptom changes
2. Stage 2 — Moderate COPD (GOLD 2)
- Characteristics: FEV1 50–79% predicted. Symptoms become more noticeable; physical activity may be limited.
- Common Symptoms: Persistent cough, increased sputum, breathlessness on exertion, occasional exacerbations.
- Treatment Approach:
- Long-acting bronchodilators (LABA or LAMA)
- Pulmonary rehabilitation programs to improve exercise capacity
- Continued emphasis on lifestyle modifications and vaccination
- Assessment for comorbid conditions
3. Stage 3 — Severe COPD (GOLD 3)
- Characteristics: FEV1 30–49% predicted. Frequent exacerbations, more pronounced activity limitation.
- Common Symptoms: Severe dyspnea with daily activities, chronic cough, fatigue, recurrent infections.
- Treatment Approach:
- Dual or triple inhaler therapy (LABA + LAMA ± ICS)
- Consideration of new COPD treatment medications including phenotype-guided biologics for patients with persistent inflammation
- Pulmonary rehabilitation and oxygen therapy if indicated
- Close monitoring to prevent acute exacerbations
4. Stage 4 — Very Severe COPD (GOLD 4)
- Characteristics: FEV1 < 30% predicted or presence of chronic respiratory failure. Life-threatening exacerbations possible.
- Common Symptoms: Severe breathlessness even at rest, poor exercise tolerance, systemic effects (muscle wasting, weight loss).
- Treatment Approach:
- Comprehensive inhaler or injection therapy, including long-acting biologics or injectable bronchodilators for systemic control
- Long-term oxygen therapy for hypoxemia
- Advanced pulmonary rehabilitation, nutritional support, and palliative care considerations
- Evaluation for surgical interventions (lung volume reduction surgery, transplantation) in selected patients
Each stage requires a tailored treatment plan to maximize quality of life, reduce exacerbations, and slow disease progression.
With the introduction of new COPD treatment injections, dual-pathway drugs, and biologics in 2025, clinicians now have a broader arsenal to match therapies to patient phenotype and disease stage.
This staged understanding also sets the context for looking forward: what comes next after the launch of these innovative COPD therapies?
What’s Next After The New COPD Treatment Launch?
The launch of new drugs is far from the endpoint; it is, rather, the prologue to a new era.
As Dengyue has consistently observed while keeping pace with the latest global medical advancements, the treatment of Chronic Obstructive Pulmonary Disease (COPD) is profoundly integrating with big data, artificial intelligence, and biotechnology.
This convergence is driving a parallel evolution toward a “predictable, preventable, and personalized” era of precision medicine on both global and Chinese stages.
🌐 From a global perspective, the therapeutic paradigm is undergoing a deep transformation.
Drawing from the most recent developments, precision medicine is moving from concept to clinical practice.
- The ultra-long-acting biologic Depemokimab is currently undergoing Phase III clinical trials in China, including at leading centers such as West China Hospital of Sichuan University, targeting COPD patients with type 2 inflammation and showcasing the potential of a “biannual injection” frontier therapy.
- The latest 2025 GesEPOC guidelines from Spain emphasize guiding treatment decisions based on biomarkers like blood eosinophil counts, signifying that precision phenotyping has become the international standard of care.
- Innovative therapies for non-type 2 inflammation (such as treatments targeting extracellular DNA) are also being explored.
In the context of Chinese practice, this global trend is synergizing with the “people’s health-centered” healthcare system reform, accelerating implementation through three key pathways:
- Technology-Empowered Primary Care—Exemplified by the pioneering establishment of “Digital Therapy Centers for Chronic Respiratory Diseases” in cities like Wuhan and Tianjin.
- Reimbursement-Driven Innovation—The dynamic adjustment mechanism of the National Reimbursement Drug List (NRDL) is accelerating the clinical adoption of innovative therapies.
- Data-Informed Decision Making—Collecting data on the actual efficacy and safety of innovative drugs within the Chinese context will generate robust “Chinese evidence,” informing clinical guidelines and reimbursement policies to achieve genuine value-based healthcare.
In summary, global scientific breakthroughs and China’s systemic innovations are merging into a powerful force.
As HongKong DengYue Medicine firmly believes, tracking cutting-edge medical advances has one ultimate goal: to serve clinical practice and patients.
🙂 By empowering primary care with technology, guiding innovation through reimbursement, and optimizing decisions with data, we are steadily moving toward building a comprehensive prevention and treatment system for chronic respiratory diseases that covers the entire population and the full life cycle.
This progress ensures that every individual living with COPD can enjoy the freedom and quality of breath they deserve.
FAQ about New COPD Treatment Launched
How much does ensifentrine cost?
US list price: Around $2,950 per month.
Other countries: Prices vary; not widely available yet.
What stage of COPD is anoro used for?
All patients at GOLD stages 2-4, according to GOLD classification at the time of study.
ANORO was studied in patients with moderate or worse COPD.
Which is better, Trelegy or Breztri?
Metered-dose inhaler budesonide-glycopyrrolate-formoterol (Breztri Aerosphere) was associated with a higher risk of a first moderate or severe COPD exacerbation.
When will ensifentrine be available?
United States: Approved by the FDA in June 2024 and available since around August 2024.
Macau (China): Approved and available.
Europe/UK: Not yet approved; availability timing is uncertain.