What Causes Plaque Psoriasis? How Does the New Drug Mufemilast Offer a Novel Treatment Choice?
🤔 When well-defined red patches covered in silvery-white scales appear on the skin, it is often more than just a cosmetic concern—it reflects a “microscopic war” being waged on the skin’s surface.
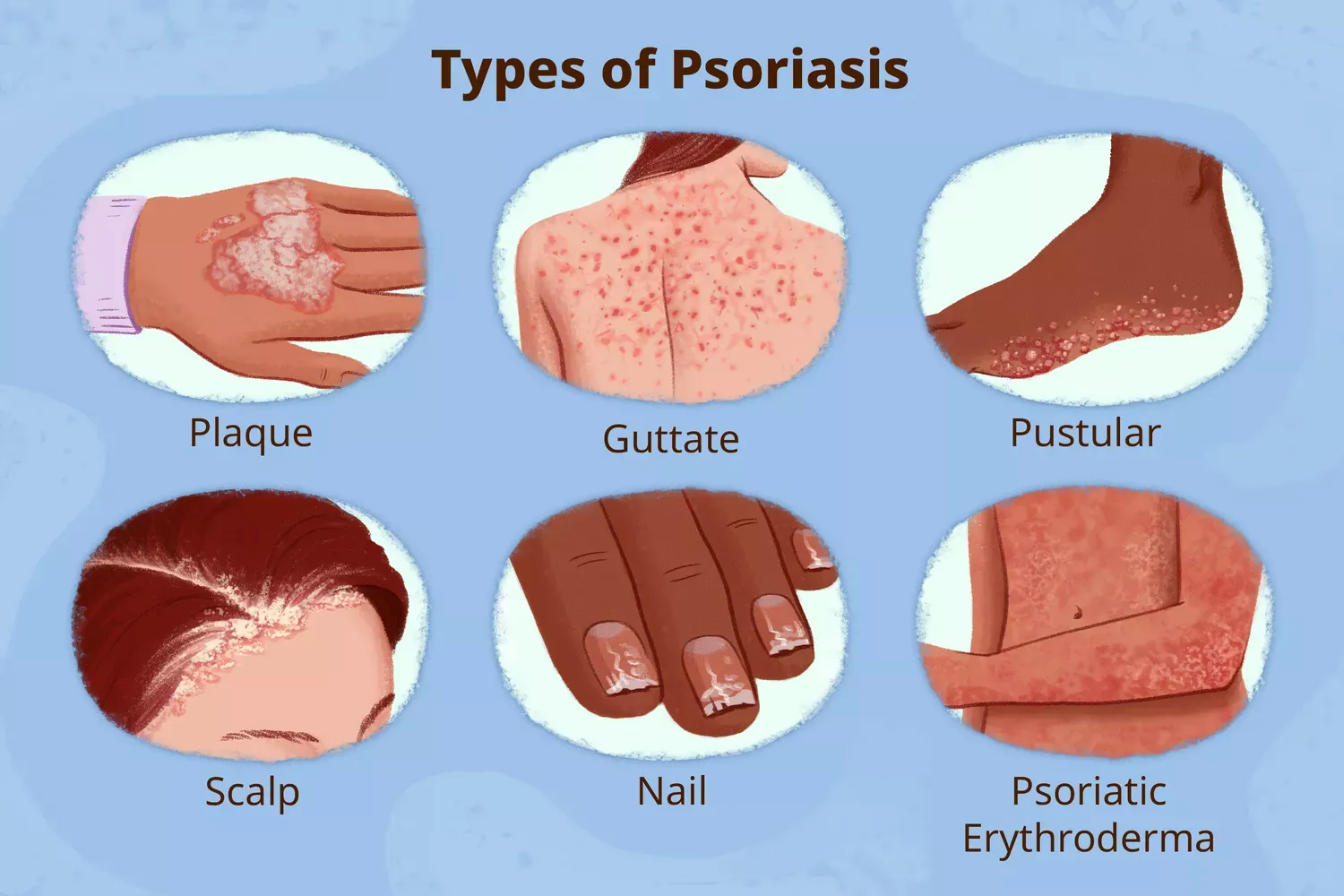
Plaque psoriasis is a chronic immune-mediated inflammatory skin disease and the most common form of psoriasis. This disease affects approximately 1–3% of the global population, with an estimated 6 million patients in China.
So, what causes plaque psoriasis?
👉 In short, the cause of plaque psoriasis lies not in the skin itself, but in the immune system. It is a chronic inflammatory disease in which the immune system mistakenly attacks the body’s own skin, requiring long-term management and treatment.
Traditional treatments have struggled to balance efficacy, safety, and convenience, leaving patients caught in a cycle of recurrent flare-ups and treatment side effects.
However, in October 2025, the approval of Mufemilast Tablets by the National Medical Products Administration (NMPA) introduced a novel treatment option for patients.
✨ DengYue Medicine will delve into the underlying mechanisms of this disease and explain how this newly available therapeutic option, now efficiently distributed across China, provides a novel and promising treatment choice for patients.
Understanding the “Opponent”—What Is Plaque Psoriasis?
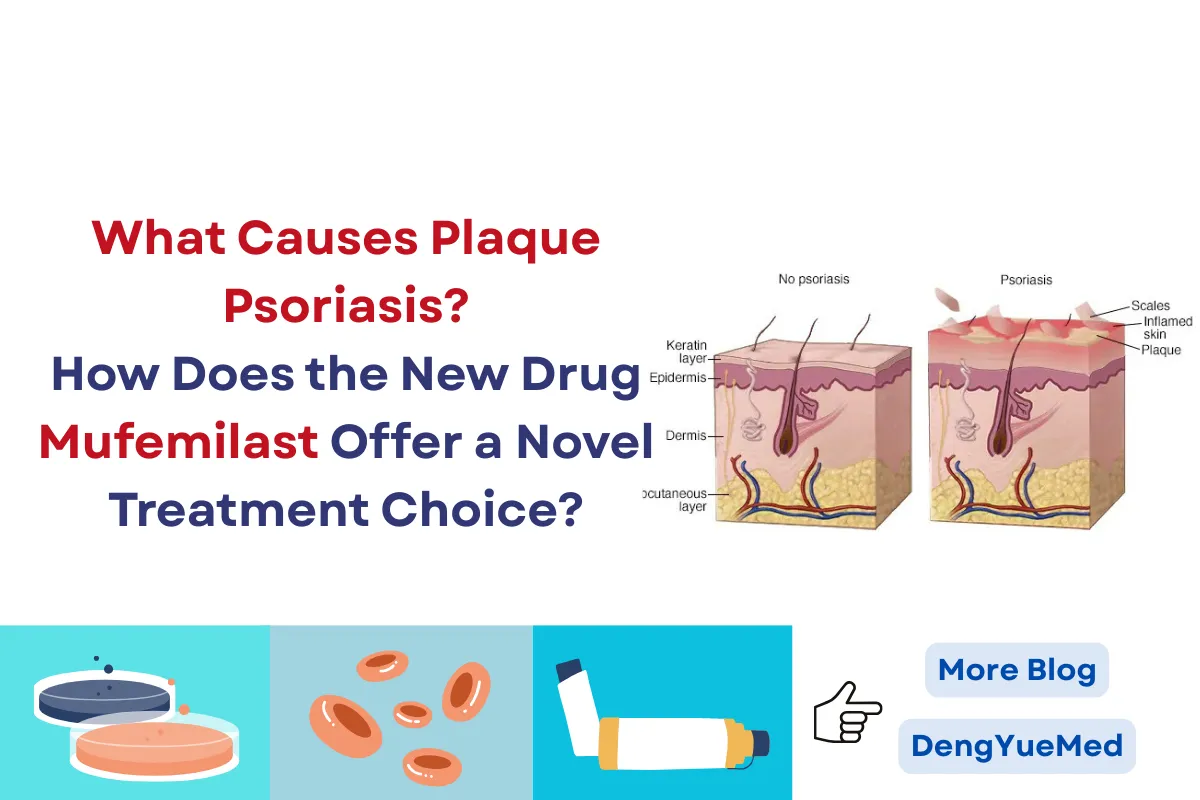
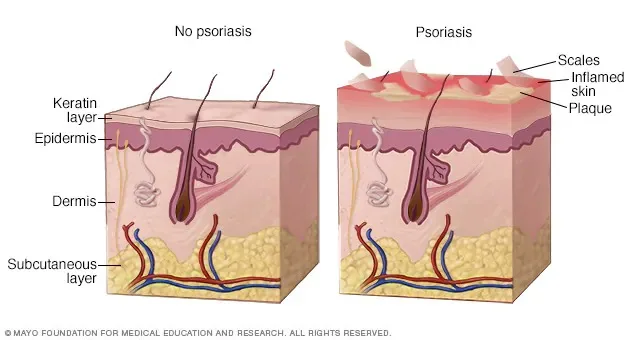
Imagine the normal “life cycle” of a skin cell takes about 28-30 days, gradually migrating from the basal layer to eventually shed naturally from the stratum corneum.
However, in patients with plaque psoriasis, this process is accelerated to a mere 3-4 days.
This abnormal acceleration does not originate from the skin itself but stems from “erroneous signals” from the immune system.
Research shows that specific immune cells (such as Th17 cells) in psoriasis patients are abnormally activated, secreting large quantities of inflammatory factors like IL-17 and IL-23.
These factors act as incorrect “accelerator signals,” prompting excessive proliferation of keratinocytes.
This process creates a vicious cycle: inflammation leads to skin hyperplasia, and the hyperplastic skin, in turn, releases more inflammatory signals, directly explaining what causes plaque psoriasis and its characteristic symptoms.
👉 Understanding this immune-driven process helps explain why plaque psoriasis is persistent, recurrent, and difficult to control with surface-level treatments alone.
Typical Presentation: “Maps and Frost” on the Skin
Visual Triad:
- Erythema: Well-defined red patches that blanch temporarily with pressure.
- Elevation: Noticeably thicker than surrounding healthy skin, firm to the touch.
- Scaling: Surface covered with layers of dry, silvery-white scales. Gentle scraping reveals the characteristic “candle-wax phenomenon,” “film phenomenon,” and “Auspitz sign” (pinpoint bleeding).
Distribution Pattern:
These lesions show a preference for specific sites, appearing in approximately 75-90% of patients:
- Extensor surfaces of elbows (85%)
- Knees (70%)
- Lumbosacral area (50%)
- Scalp (50-80%)—What causes plaque psoriasis on the scalp involves the same immune mechanisms, with inflammation triggering rapid cell turnover in hair follicles, leading to thick, scaly plaques that may extend beyond the hairline.
- Nails (25-50%, manifesting as pitting or onycholysis)
From “Mild” to “Moderate-to-Severe”: A Quantitative Change Leading to a Qualitative Shift
Clinicians use various tools to assess disease severity:
- Body Surface Area (BSA) Rule: The area of one palm (including fingers) roughly equals 1% of BSA. Involvement exceeding 10% (more than ten palm-sized areas) is typically classified as moderate-to-severe.
- Psoriasis Area and Severity Index (PASI): Comprehensively evaluates lesion area, erythema, induration, and scaling. A PASI score ≥ 12 is often the threshold for moderate-to-severe disease.
- Impact on Quality of Life: Even with limited skin involvement, if the disease significantly affects daily life, work, social interactions, or mental health (DLQI > 10), active treatment is equally necessary. This holistic assessment is part of modern plaque psoriasis treatment strategies.
The Invisible Burden: Dual Pressure—Physical and Psychological
Physical Burden:
- Pruritus (Itching): About 70-90% of patients experience moderate-to-severe itching, with 40% suffering from sleep disturbances as a result.
- Pain: Cracking plaques cause pain in approximately 30% of patients.
- Comorbidity Risk: As mentioned, patients have an increased risk of metabolic syndrome and cardiovascular diseases.
Psychosocial Burden:
😣 Surveys indicate that over 50% of psoriasis patients experience anxiety or depressive symptoms, and 40% avoid social activities due to their skin lesions.
This “invisible scar” often impacts patients’ quality of life more profoundly than the physical lesions themselves.
🏃♂️➡️ Recognizing plaque psoriasis as a systemic immune-mediated disease—driven by specific plaque psoriasis causes and manifesting with characteristic plaque psoriasis symptoms—is the first step.
The next crucial question becomes: How do we intervene in this complex process?
For decades, the medical community has been developing and refining a therapeutic arsenal to combat this condition, each with its own strengths and limitations.
As we move from understanding what causes plaque psoriasis to exploring plaque psoriasis treatment options, we will examine how therapeutic strategies have evolved to address not just the symptoms, but the root causes of this challenging disease.
The Evolution and Challenges of the Treatment “Arsenal”
An ideal treatment should simultaneously fulfill three criteria: proven efficacy, good safety, and convenient use.
😐 However, traditional therapies often only address one or two aspects, creating significant challenges in managing plaque psoriasis treatment effectively.
Traditional Therapies
- Topical Medications: The Limits of Local Control
- Corticosteroids: Provide rapid anti-inflammatory action, but long-term use can easily lead to skin atrophy and telangiectasia.
- Vitamin D3 Analogs: Safer but have a slower onset of action.
- Practical Dilemma: While effective for localized lesions, they become impractical when the affected area exceeds 10% BSA, with increased difficulty in application and risk of systemic absorption.
- Phototherapy: Balancing Time and Risk
- Narrowband UVB can achieve efficacy rates of 60-70% in treating plaque psoriasis symptoms.
- It requires hospital visits 2-3 times per week for several months, leading many patients to discontinue due to the high time commitment.
- Long-term treatment carries cumulative dose concerns and is associated with skin cancer risk.
- Traditional Oral Systemic Therapies: The Trade-off Between Efficacy and Monitoring
- Methotrexate: Proven efficacy (PASI 75 response rate ~40-60%), but requires regular monitoring of liver function and blood counts. Approximately 30% of patients discontinue due to side effects.
- Cyclosporine: Rapid onset but carries a high risk of nephrotoxicity, usually reserved for short-term use.
- Acitretin: Effective for pustular psoriasis but is teratogenic, contraindicated in women of childbearing potential.
These medications act like “broad-spectrum bombardments,” suppressing abnormal immune responses while also affecting normal bodily functions.
Biologics
The early 21st century saw biologics targeting specific inflammatory factors revolutionize plaque psoriasis treatment:
- Efficacy Leap:
- TNF-α inhibitors (e.g., adalimumab): PASI 75 response rates up to 70-80%.
- IL-17 inhibitors (e.g., secukinumab): PASI 75 response rates up to 80-90%.
- IL-23 inhibitors: Offer long-lasting effects, with some patients requiring injections only every few months.
- Practical Thresholds:
- 💉 Administration Route: Requires subcutaneous or intravenous injection; self-injection can involve pain or needle phobia.
- 💰 Financial Burden: Annual treatment costs remain substantial (thousands to tens of thousands of RMB) even after insurance reimbursement.
- 🦠 Infection Risk: Requires screening for latent infections like tuberculosis and hepatitis B.
- 🙂 Accessibility: Often unavailable in primary care settings, necessitating visits to large medical centers.
“We need a treatment that is as precise as biologics, as convenient as traditional oral drugs, and as safe as topicals.”
This common sentiment among patients reveals a long-standing treatment gap in addressing what causes plaque psoriasis: an effective, safe, convenient, and accessible oral targeted therapy.
✨ This gap represents the next frontier in plaque psoriasis medication development—a solution that directly targets the immune dysregulation at the root of the disease while overcoming the practical limitations of current options.
Spotlight on the Domestically Developed Innovative Drug Mufemilast Tablets
On October 11, 2025, an approval document from the National Medical Products Administration (NMPA) brought a brand-new choice to Chinese psoriasis patients:
The domestically developed Class 1 innovative drug Mufemilast Tablets were approved for marketing via a priority review pathway.

✅ Obtaining priority review status signifies regulatory recognition of the drug’s significant clinical value and its ability to meet an unmet medical need in plaque psoriasis treatment.
Innovative Mechanism: The “Precision Regulator” Inside Cells
Mufemilast is a highly selective phosphodiesterase 4 (PDE4) inhibitor. To understand its innovation in addressing what causes plaque psoriasis, we need to look inside the cell:
Within immune cells, cAMP (cyclic adenosine monophosphate) is a key “anti-inflammatory messenger.”
- High levels of cAMP can inhibit the production of inflammatory factors.
- The PDE4 enzyme’s role is to “break down” cAMP.
In psoriasis patients, this balance is disrupted—a core aspect of what causes plaque psoriasis.
By precisely inhibiting the PDE4 enzyme, Mufemilast effectively increases intracellular cAMP levels, acting as follows:
- Lowers the volume of pro-inflammatory factors: Reduces “inflammatory noise” from factors like TNF-α, IL-17, IL-23.
- Enhances anti-inflammatory signals: Boosts expression of anti-inflammatory cytokines.
- Multi-pathway modulation: Simultaneously influences keratinocyte proliferation and immune cell activation.
Unlike the “broad-spectrum suppression” of traditional drugs, this mechanism is more akin to conducting “precision tuning” inside the cell, directly targeting the immune dysregulation that underlies plaque psoriasis causes.
Key Data: Efficacy Beyond Theory
A Phase III clinical trial involving Chinese patients with moderate-to-severe plaque psoriasis provides solid evidence for Mufemilast Tablets:
Core Efficacy Data (Week 16 of Treatment):
- PASI 75 Response Rate: Mufemilast group 53.6% vs. placebo group 16.0% (P < 0.001)
- Clear or Almost Clear Skin (sPGA 0/1): 41.2% vs. 9.8%
- Significant Itch Improvement (Itch NRS reduction ≥ 4 points): 45.1% vs. 17.2%
Interpreting the Numbers:
- Over half of the patients achieved significant improvement in their plaque psoriasis symptoms, a competitive efficacy profile among oral targeted therapies.
- Synchronous improvement in quality of life: Rapid relief of itching directly impacts sleep and daily activities.
- Onset and maintenance: Most patients begin to see effects within 4–8 weeks, with efficacy stabilizing around week 16.
Safety and Convenience: Truly Patient-Friendly Design
Safety Profile:
- Common Adverse Reactions: Mostly mild and transient, including diarrhea (15.3%), nausea (8.7%), headache (6.2%).
- Compared to traditional oral drugs: No need for routine monitoring of liver/kidney function or blood counts; no risk of bone marrow suppression.
- Compared to biologics: No risk of tuberculosis reactivation; significantly lower infection risk.
Breakthrough in Convenience:
- Oral administration, twice daily, can be done at home.
- No injection pain or injection site reactions.
- No cold-chain storage requirements, easy to carry and use.
A Beacon of Domestic Innovation: Breaking Monopoly, Improving Access
Prior to the launch of Mufemilast Tablets, the Chinese market for oral PDE4 inhibitors had only one imported drug, apremilast.
The approval of Mufemilast marks a breakthrough for domestically developed drugs targeting this mechanism.
Domestic innovation brings not just diversity of choice but also, through market competition and medical insurance negotiations, the potential to ultimately reduce patients’ annual treatment costs, benefiting a larger population seeking effective plaque psoriasis medication.
Mufemilast Tablets offer a unique treatment choice for patients with moderate-to-severe plaque psoriasis:
Particularly suitable for:
- Patients new to systemic treatment who wish to avoid the monitoring burden of traditional drugs.
- Patients who fear or find injections inconvenient for biologics.
- Patients needing to balance efficacy with long-term safety in their plaque psoriasis treatment.
- Patients seeking better pharmacoeconomic value.
It occupies a precise position in the treatment ladder—between traditional oral drugs and biologics—filling the market gap for an effective, safe, convenient, and accessible oral targeted therapy.
Beyond Psoriasis: Broader Therapeutic Horizons
The development of Mufemilast does not end with psoriasis. Its mechanism of action, which targets fundamental inflammatory pathways, grants it potential across a spectrum of inflammatory conditions:
- Behçet’s Disease: Already in Phase III clinical trials for oral ulcers and skin lesions.
- Psoriatic Arthritis: Clinical trials are ongoing, with potential to improve joint symptoms.
- Atopic Dermatitis: Early research indicates effectiveness in controlling pruritus (itching).
This “one drug, multiple indications” development strategy not only maximizes the drug’s value but also brings hope to patients suffering from various immune-mediated inflammatory diseases.
It underscores a deeper understanding of shared plaque psoriasis causes and pathways across different conditions, paving the way for more versatile and effective plaque psoriasis medication options in the future.
Looking to the Future — How Should Patients Proceed?
There is no “one-size-fits-all” solution in plaque psoriasis treatment.
While Mufemilast Tablets represent a new option, each patient’s situation is unique. Treatment decisions must be based on:
- Disease Assessment: Lesion area, location, and symptom severity of plaque psoriasis symptoms.
- Individual Factors: Age, comorbidities, fertility plans, and lifestyle.
- Treatment History: Previous treatment responses and tolerance.
- Economic Considerations: Drug accessibility and ability to pay.
Patient-Doctor Communication Checklist: Key Questions to Discuss
❓ If considering Mufemilast Tablets, it is advisable to prepare the following questions for discussion with your dermatologist:
- “Does the severity of my condition meet the indication criteria for this plaque psoriasis medication?”
- “What are the expected benefits compared to my current or past plaque psoriasis treatment?”
- “What are the common side effects, and how are they managed?”
- “How long does it take to start working, and how is effectiveness evaluated?”
- “How long is treatment typically continued? What happens if treatment is stopped?”
- “Is this medication available at local pharmacies? What is the current insurance coverage policy?”
Conclusion
The “root cause” of plaque psoriasis is deeply embedded in the complex regulatory network of the immune system.
Our understanding and treatment of it have evolved from focusing on surface manifestations to the underlying essence, and from broad approaches to precise interventions.
💊 The emergence of Mufemilast Tablets marks a significant milestone, signifying that China has progressed from “following” to “running alongside” and even achieving partial leadership in the field of autoimmune disease treatment.
This innovation is more than just a molecular formula from the laboratory—it is a bridge connecting scientific breakthroughs with clinical needs.
It aims not only to alleviate plaque psoriasis symptoms but also to restore patients’ quality of life and dignity.
In the era of precision medicine, we now possess more advanced tools to target the very plaque psoriasis causes that drive this challenging condition.
Treatment options have never been so diverse, and the patient’s voice has never been so crucial.
In this age of shared decision-making between doctors and patients, understanding the disease, knowing the available plaque psoriasis treatment options, and engaging in proactive communication are essential first steps for every patient on the path to better health.
As key contributors to healthcare accessibility, distributors like Hong Kong DengYue Medicine play a vital role in this new era.
🙂 As global drug wholesale distributor, through our nationwide pharmaceutical distribution network, we have been instrumental in accelerating the accessibility of this groundbreaking treatment
FAQ about What Causes Plaque Psoriasis
Why do I suddenly have plaque psoriasis?
No one knows exactly what causes them.
Common plaque psoriasis triggers may include: Certain foods or drinks.
Certain prescription medications (like lithium and beta-blockers).
What is the main cause of psoriasis?
Psoriasis occurs when skin cells are replaced more quickly than usual.
It’s not known exactly why this happens, but research suggests it’s caused by a problem with the immune system.
What is the rule of 9 in psoriasis?
The rule of 9 is a method used by clinicians to estimate how much of the body surface area is affected by psoriasis.
What foods should I avoid with psoriasis?
Foods with saturated fats and trans fats.